What is Gonorrhea? STD, Sign & Symptoms, Treatment
What is Gonorrhea?
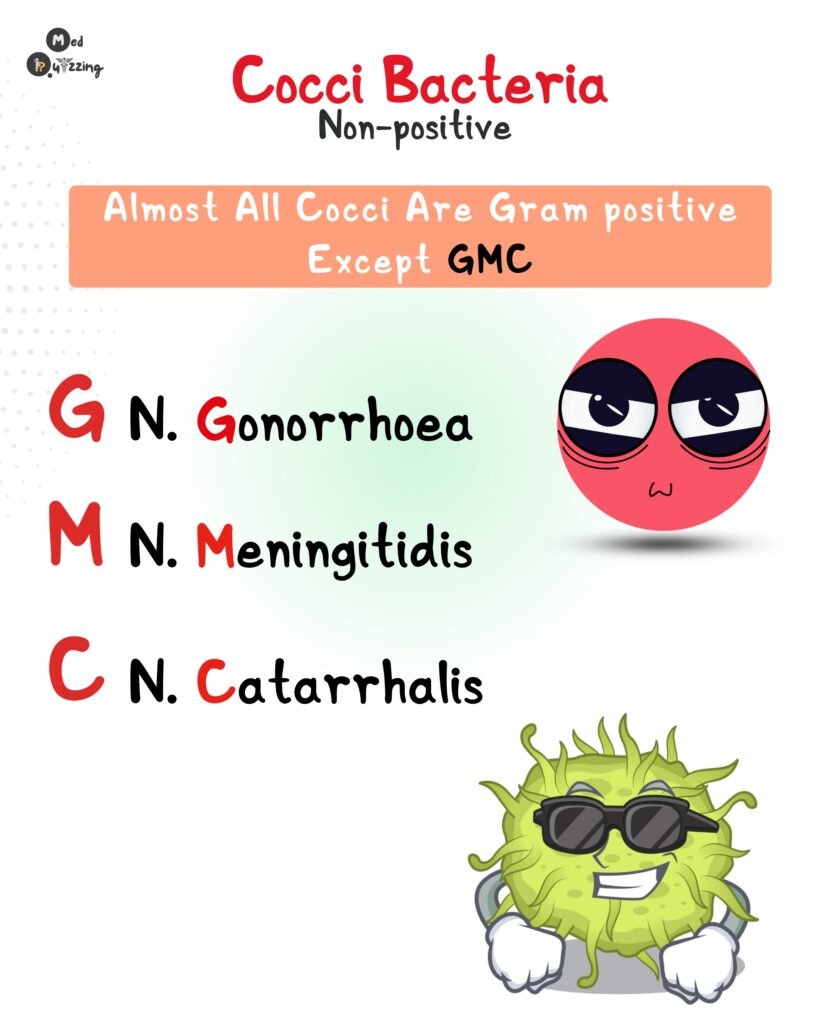
Gonorrhea is an STI caused by the gram-negative bacterium Neisseria gonorrhoeae. Microscopically, this bacterium appears as paired, round cells enclosed within a capsule—a formation known as diplococci.
A handy way to recall its classification: the word “gonorrhea” contains a “G” and “N” close together, which can help remind you it’s Gram-negative Neisseria.
How is Gonorrhea Transmitted?
Gonorrhea is typically spread through unprotected sexual contact, including vaginal, oral, or anal intercourse with an infected partner. However, it can also be passed from mother to baby during delivery. In such neonatal cases, the infection may result in:
- Premature birth
- Eye infections, which, if untreated, can lead to blindness
- Meningitis in severe cases
This makes prenatal screening and timely treatment essential during pregnancy.

Signs and Symptoms: Think “CLAP“
To make symptom recognition easier, remember the mnemonic “CLAP”, a nickname often used for gonorrhea:
- C – Conjunctivitis: Particularly dangerous for newborns who may develop eye infections after passing through an infected birth canal.
- L – Lack of Symptoms: Especially in women. Gonorrhea may silently mimic urinary tract or vaginal infections, making it harder to detect.
- A – Abnormal Discharge: Thick, yellow-green discharge may appear from the penis, vagina, or anus, depending on the infected site.
- P – Pelvic Inflammatory Disease (PID): If untreated, gonorrhea can spread to the uterus, ovaries, and fallopian tubes, leading to infertility, chronic pelvic pain, or ectopic pregnancy.
Additional symptoms include:
- Pain or burning during urination
- Tender, swollen testicles in males
- Localized swelling in the throat, rectum, or genitals—whichever site was exposed
Treatment and Management of Gonorrhea
1. Antibiotic Therapy
Since gonorrhea is caused by a gram-negative bacterium, treatment involves antibiotic therapy. The CDC currently recommends:
- A single intramuscular dose of ceftriaxone for non-pregnant individuals with uncomplicated gonorrhea.
- If chlamydia hasn’t been ruled out, add doxycycline (unless contraindicated).
⚠️ Note: Previous guidelines used dual therapy with ceftriaxone and azithromycin, but this has been updated due to resistance concerns.
For pregnant patients, the treatment remains similar, except doxycycline should be avoided. An alternative antibiotic will be used if chlamydia co-infection is suspected, as doxycycline can affect fetal bone and tooth development.
2. Patient Education
Comprehensive education is vital to ensure recovery and prevent reinfection. Key points include:
- Avoid all sexual activity for at least 7 days after completing treatment and until symptoms fully resolve.
- Use barrier methods (like condoms) upon resuming sexual activity.
- All recent sexual partners should be notified, tested, and treated.
- Follow-up testing is advised within 3 months to confirm the infection has cleared or detect reinfection.
Monitoring:
- Screening: Routinely assess for symptoms, especially in high-risk groups such as sexually active individuals under age 25 or those with multiple partners.
- Testing: Urine samples or swabs from affected sites are used to confirm infection. Because gonorrhea often co-exists with chlamydia, both are typically tested together.
- Education: Teach patients the importance of abstaining from sex until treatment is complete, and symptoms have resolved.
- Partner Notification: Encourage patients to inform their sexual partners to get tested and treated to prevent reinfection.
The CDC recommends annual testing for sexually active individuals under 25 and for pregnant patients during their first prenatal visit, and again in the third trimester if they are at high risk.