What is Cholecystitis? symptoms, causes & treatment
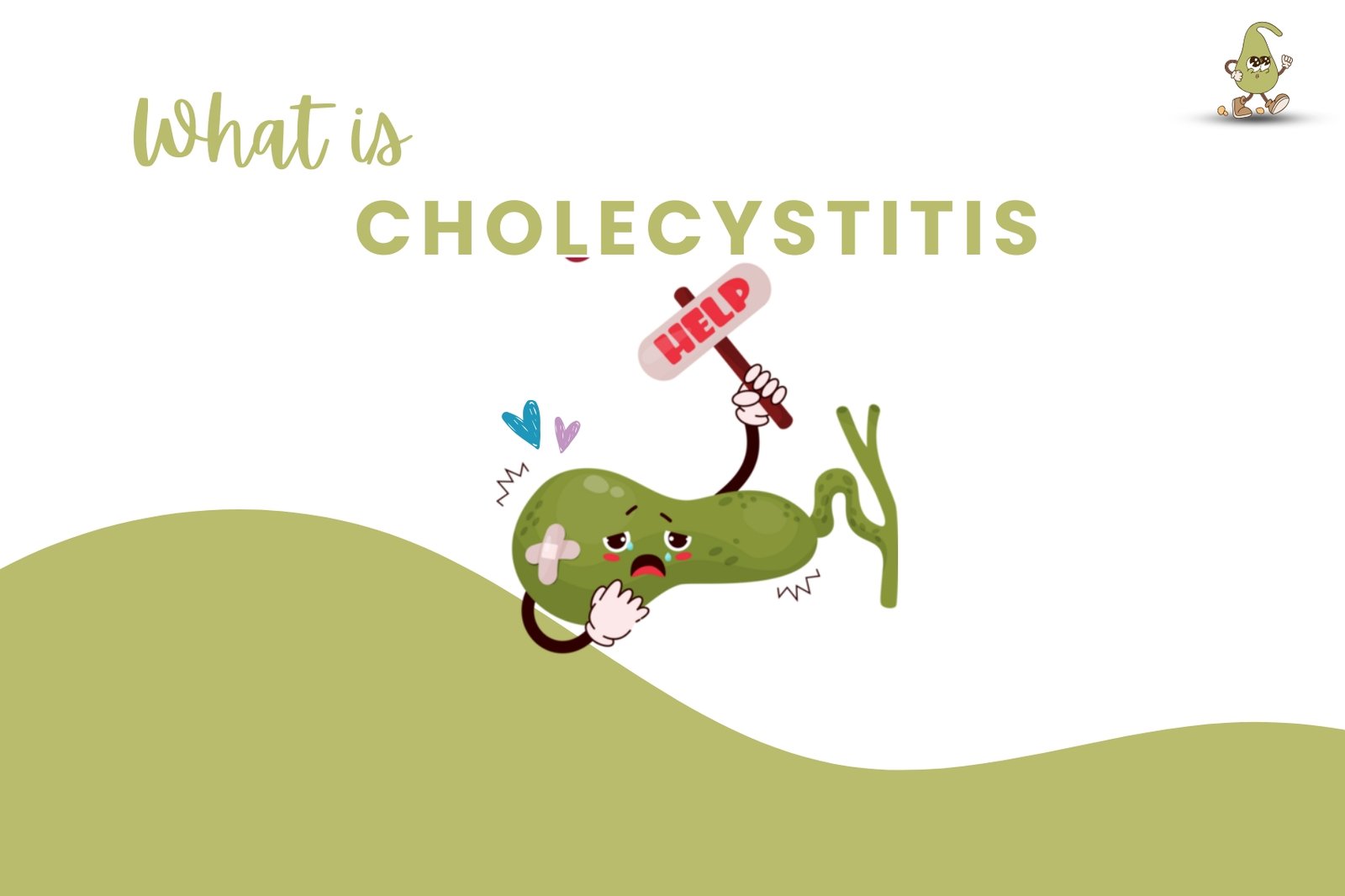
What is Cholecystitis?
To understand cholecystitis, let’s break the word apart. The word “chole” means bile, “cyst” means membranous sac, and “itis” means inflammation.
So, cholecystitis refers to inflammation of the membranous sac that holds bile. What structure in the body does that? The gallbladder. Cholecystitis is inflammation of the gallbladder.
Now, to help us understand this condition, we need to talk about the role of the gallbladder. Your gallbladder is a unique-looking structure—it’s round, pear-shaped, and green. It’s found on the right side of the body, just beneath the liver, which is fitting because the liver and gallbladder work together. Both share their love for a substance called bile. The liver creates bile, which then leaves the liver, travels down the hepatic duct, and enters the gallbladder, where it’s stored and concentrated.
What is Bile?
Bile is an important substance that helps us digest fats, including fat-soluble vitamins like A, D, E, and K. It also serves as a vehicle for bilirubin to exit the body through stool.
Let’s see how bile works to digest fats. When you eat a meal, the food goes into your stomach, where it’s partially digested. Once it leaves the stomach, the food becomes chyme—a thick, semi-pulpy substance containing gastric juices and fats. This chyme travels to the small intestine and enters the duodenum. Here, a duct senses the fat in the chyme and signals the gallbladder to contract, releasing bile through the cystic duct and common bile duct into the duodenum to assist with fat digestion.
If there’s an issue with the gallbladder—such as an obstruction from a gallstone or dysfunction due to trauma—the bile can’t leave the gallbladder to aid digestion. As a result, the fats in the chyme won’t be digested, and the patient will excrete them. This leads to greasy, fatty stools called steatorrhea, a common sign in patients with cholecystitis, especially chronic cases.
Bile also helps bilirubin exit the body through stool. Bilirubin is a substance created when old, worn-out red blood cells break down. It’s brownish-orange in color and gives stool its characteristic brown color. If the gallbladder is inflamed and bile can’t reach the small intestine, bilirubin can’t exit the body. This can cause jaundice, where bilirubin leaks into the tissues, turning the sclera of the eyes and skin yellowish-orange. The stool may also appear clay-colored, and the urine may become dark.
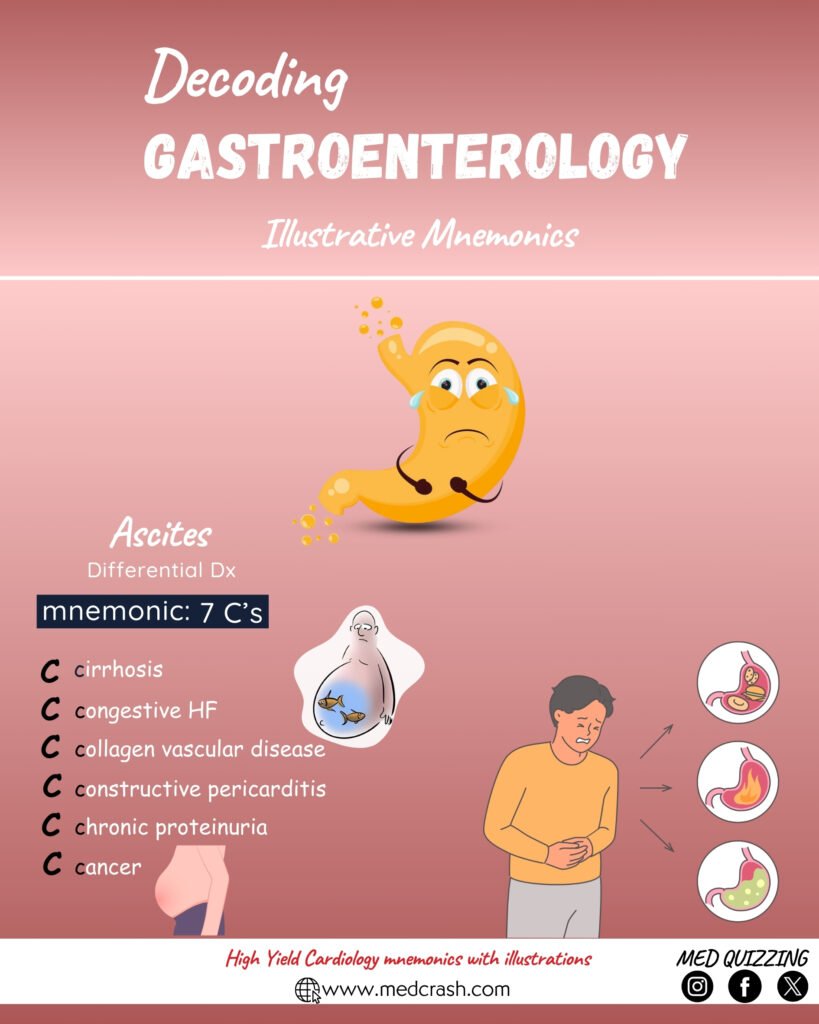
Causes of Cholecystitis
What causes the gallbladder to become inflamed? One of the main causes is obstruction, such as a blockage in the cystic duct that prevents bile from leaving the gallbladder. Another common cause is gallstones, which are often linked to risk factors like being female, obese, over 40, having a family history of gallstones, being pregnant, or being of Native American or Mexican American ethnicity.
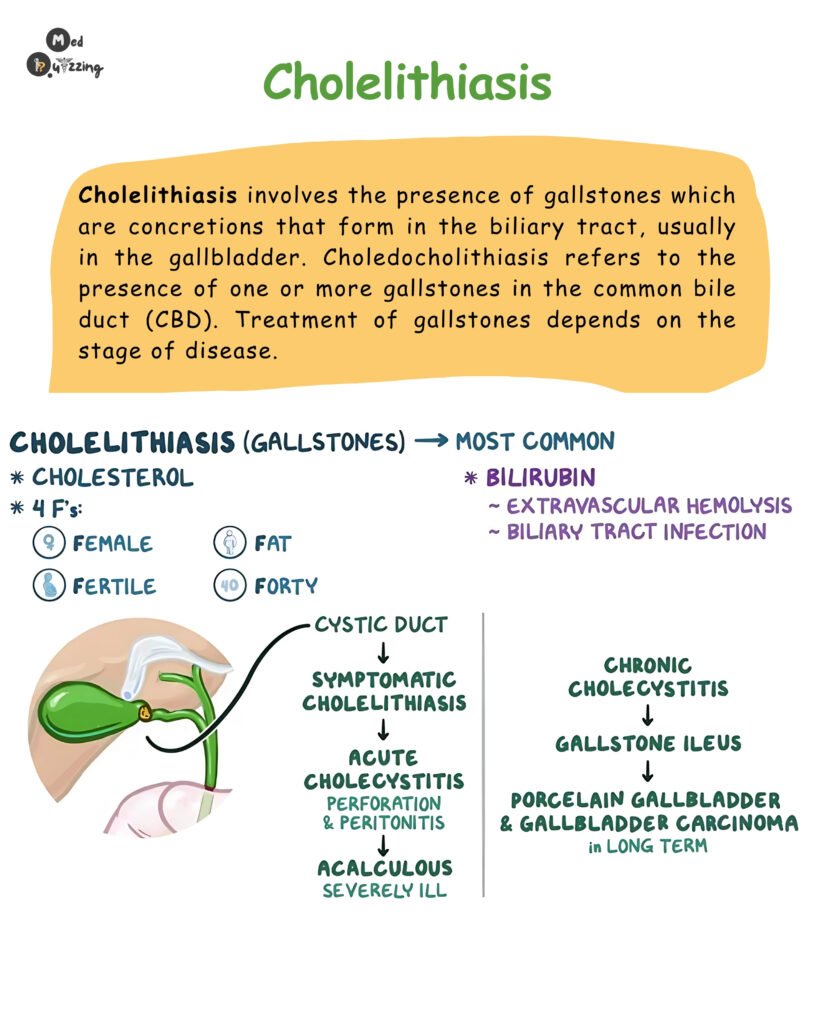
Another cause is acalculous cholecystitis, which occurs without gallstones. This happens when the gallbladder isn’t functioning properly, often due to severe illness, trauma, burns, sepsis, or prolonged use of total parenteral nutrition (TPN).
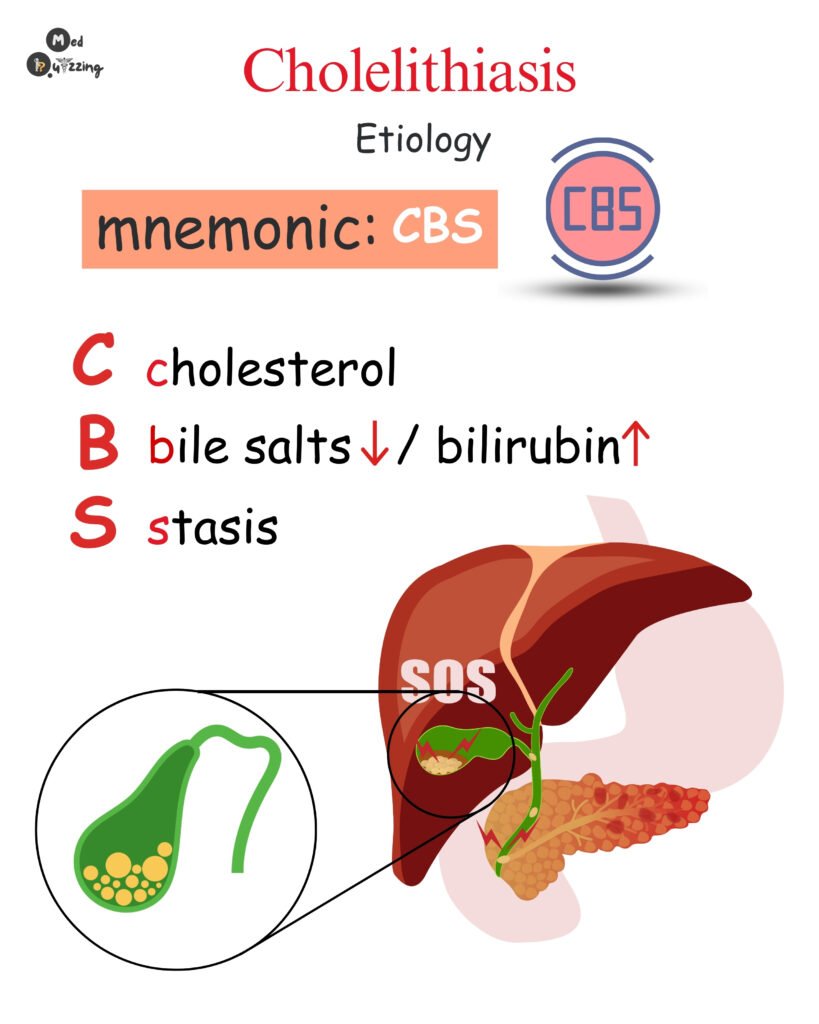
In these cases, the gallbladder doesn’t contract as it should, causing bile to stagnate, thicken, and increase pressure within the gallbladder. This inflames and damages the gallbladder wall, leading to swelling and potential complications like hepatitis, bile duct infections, pancreatitis, sepsis, or even gallbladder rupture.
Signs and Symptoms of Cholecystitis
Patients with cholecystitis often experience:
- Nausea and vomiting: Severe enough to require a nasogastric tube for GI decompression.
- Dehydration: Due to persistent vomiting, patients may need IV fluids.
- Pain: Intense abdominal pain, often in the epigastric region, which may radiate to the right scapula or shoulder blade. The pain can worsen after eating a heavy, greasy meal.
- Positive Murphy’s sign: During palpation of the gallbladder area, the patient may stop breathing due to pain.
- Bloating, fever, and increased heart rate: Common systemic symptoms.
- Jaundice, dark urine, and clay-colored stools: Signs of bilirubin buildup due to bile obstruction.
- Steatorrhea: Greasy, fatty stools from undigested fats.
Diagnosis of Cholecystitis
To diagnose cholecystitis, physicians may order:
- Abdominal ultrasound: To visualize the gallbladder and detect gallstones or inflammation.
- HIDA scan: A radioactive tracer is injected to assess gallbladder function.
- CT scan: To evaluate the gallbladder and surrounding structures.
Treatment Options for Cholecystitis
- ERCP (Endoscopic Retrograde Cholangiopancreatography): A procedure to remove gallstones from the bile duct using an endoscope.
- Cholecystectomy: Surgical removal of the gallbladder often performed laparoscopically. After surgery, bile flows directly from the liver to the duodenum.
Post-Surgical Care
After a cholecystectomy:
- Monitor for infection at incision sites.
- Manage pain, including shoulder pain from laparoscopic carbon dioxide insufflation.
- Encourage early ambulation, coughing, deep breathing, and incentive spirometry use.
- Provide T-tube care if applicable, ensuring proper drainage and monitoring for complications.