What is Systemic lupus erythematosus (SLE)? Symptoms, Causes
What is Systemic lupus erythematosus (SLE)?
Systemic lupus erythematosus (SLE), commonly known as lupus, is a chronic autoimmune disease that causes inflammation in various organs, tissues, and joints. This inflammation can lead to permanent damage if left untreated. Lupus affects individuals differently—some may experience mild symptoms, while others face severe complications. Commonly affected areas include the skin, joints, kidneys, brain, heart, lungs, and blood system.
Lupus is characterized by periods of flare-ups (when symptoms are active) and remission (when symptoms subside). This unpredictable nature makes diagnosis challenging, requiring a thorough evaluation of the patient’s medical history, family history, symptoms, and lab results. While there’s no cure for lupus, treatments are available to manage symptoms, reduce flare-ups, and improve quality of life.
Who is at Risk?
Lupus is more common in women, particularly Black, Latina, and Asian women of childbearing age. Hormonal changes, such as those during menstruation, pregnancy, and postpartum, are believed to play a role in triggering or worsening the disease. Other risk factors include:
- Genetic predisposition: Family history of lupus or other autoimmune diseases.
- Environmental triggers: Excessive sun exposure, infections, or certain medications.
Pathophysiology:
Systemic lupus erythematosus begins at the cellular level, specifically during apoptosis (programmed cell death). Normally, when a cell becomes unhealthy, it undergoes apoptosis, breaking down into smaller fragments called apoptotic bodies. Macrophages (immune cells) then clean up these fragments.
However, in lupus, this process is disrupted. Macrophages either fail to clear the apoptotic bodies or do so too slowly. As a result, the fragments leak their contents, including nuclear material, into the body. The immune system mistakes this material for foreign invaders and produces anti-nuclear antibodies (ANAs). These antibodies form immune complexes that circulate and deposit in tissues, triggering inflammation and damage to organs and joints.
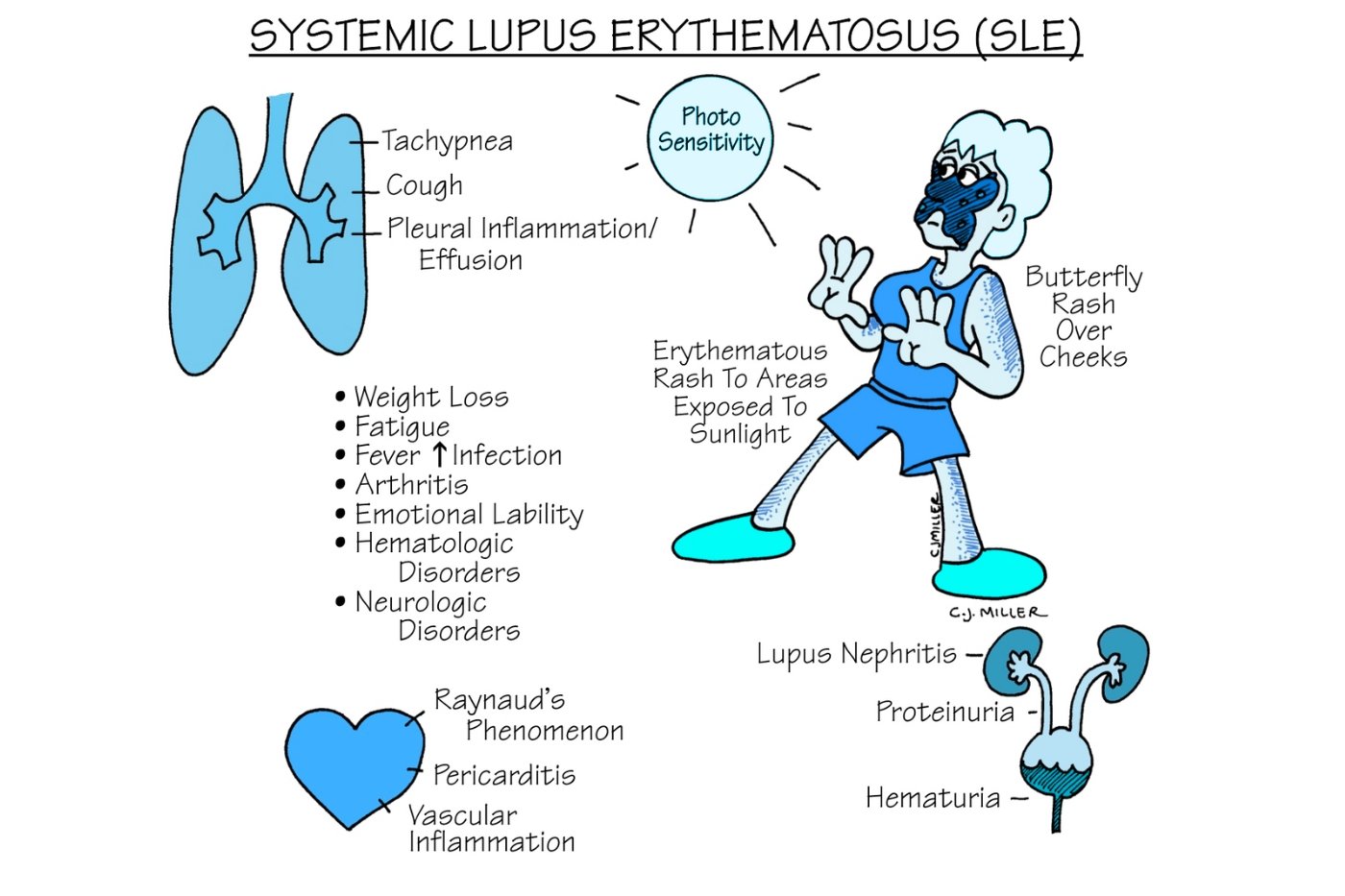
Signs and Symptoms of Lupus:

Symptoms vary depending on the affected area:
- Brain: Fatigue, memory loss, mood changes, seizures.
- Skin: Sunlight-triggered rashes (butterfly or disc-shaped), hair loss.
- Eyes/Mouth: Dryness, redness, mouth ulcers.
- Heart: Chest pain, inflammation, murmurs.
- Lungs: Chest pain, increased risk of pneumonia.
- Kidneys: Swelling, high blood pressure, risk of kidney failure.
- Blood: Increased infections, blood clots, anemia.
- Joints: Pain, swelling, Raynaud’s phenomenon (fingers/toes turning blue in cold).
- Pregnancy: Higher risk of flare-ups, clotting, and complications—careful planning is essential.
Diagnosing:
Diagnosis involves a combination of clinical evaluation and lab tests:
Antibody Testing
- ANA (Antinuclear Antibodies): Detects autoantibodies targeting cell nuclei.
- Anti-dsDNA (Double-Stranded DNA Antibodies): Specific to lupus; rarely found in other conditions.
- Anti-Smith Antibodies: Another lupus-specific marker.
Inflammatory Markers
- ESR (Erythrocyte Sedimentation Rate) and CRP (C-Reactive Protein): Elevated during flare-ups, indicating active inflammation.
- Complement Levels (C3, C4): Decreased due to inflammation.
Other Tests
- Complete Blood Count (CBC): Checks for anemia or low white blood cells.
- Metabolic Panel: Assesses kidney function.
Treatment:
While lupus has no cure, treatments aim to control symptoms and prevent complications:
-
Steroids
- Drugs: Prednisone, prednisolone.
- Benefits: Rapidly reduces inflammation.
- Risks: Weight gain, osteoporosis, hyperglycemia, increased infection risk. Used short-term and tapered gradually.
-
NSAIDs
- Drugs: Ibuprofen, naproxen.
- Benefits: Reduces joint pain and fever.
- Risks: Gastrointestinal issues (ulcers, bleeding), kidney concerns.
-
Antimalarials
- Drug: Hydroxychloroquine.
- Benefits: Long-term disease control by reducing antibody attacks.
- Precautions: Regular eye exams (risk of retinal damage); avoid smoking (reduces drug efficacy).
-
Immunosuppressants
- Drugs: Azathioprine, mycophenolate mofetil.
- Use: For severe cases to reduce reliance on steroids.
- Risks: Increased infection risk; avoid live vaccines.
-
Biologics
- Drug: Belimumab.
- Benefits: Reduces B-cell activity, controlling antibody production.
- Precautions: Monitor mental health (risk of depression), infection risk, and avoid live vaccines.
Pregnancy and Lupus:
- Lupus must be well-controlled for at least six months before conception.
- Pregnancy and postpartum periods increase the risk of flare-ups.
- Risks include miscarriage and complications, necessitating careful planning and monitoring.
Preventing Lupus Flares:
To minimize flare-ups, remember the mnemonic “LESS”:
- L: Lower Stress – Identify and manage stressors using relaxation techniques.
- E: Exercise – Maintain joint mobility and manage weight.
- S: Sleep – Aim for more than 8 hours to prevent exhaustion and stress.
- S: Sun Protection – Use sunscreen, wear hats, and avoid prolonged sun exposure.
Recognizing Signs of a Flare Mnemonic (FLARE)
- F: Fatigue
- L: Low-grade fever
- A: Achy joints
- R: Rashes
- E: Edema (swelling in legs and hands)