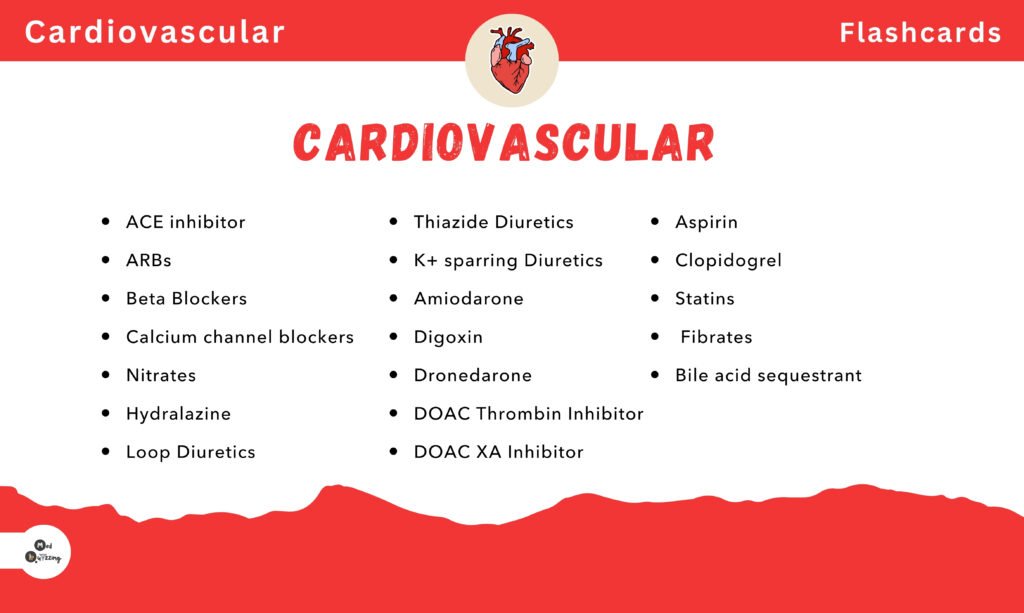
Cardiac Medications, Drugs, Side Effects, indications
Anti-Coagulants
First up is the medication class known as the anti-coagulants. The prefix “anti” means against, so we are working against coagulation—that is, the body’s ability to form a clot. We affect that process with medications such as
- Heparin
- Low molecular weight heparin
- Enoxaparin
- Warfarin
- Rivaroxaban
- Dabigatran
- Apixaban
These medications treat conditions with clotting issues, for instance, pulmonary embolism, deep vein thrombosis, atrial fibrillation, or post-surgical cases (like hip and knee surgery) to prevent clot formation after a myocardial infarction or during unstable angina.
How They Work:
They slow down the coagulation process by interrupting the clotting cascade. Importantly, these medications do not dissolve or break up existing clots; they only prevent clots from growing or new ones from forming.
Side Effects:
- Bleeding and bruising
- Upset stomach (nausea and vomiting)
- Warfarin, for example, can affect the bones (osteoporosis)
- Potential hair loss
Monitoring:
- Monitor for signs of bleeding using various tests.
- Check the complete blood count (CBC), focusing on hemoglobin and hematocrit levels for any downward trends that may indicate internal bleeding.
- For patients on heparin, monitor platelet counts for heparin-induced thrombocytopenia.
- Monitor PTT for heparin and PT/INR for warfarin.
- Assess patients for signs of bleeding, such as pink-tinged urine, dark sticky stools, oozing gums, pain (especially in the head or stomach), decreasing blood pressure with increasing heart rate, and heavy menstrual bleeding.
Antiplatelets
Next are the antiplatelets, which work against platelet aggregation—the clumping of platelets that can lead to clot formation. Medications in this class include
- Aspirin
- Clopidogrel
- Cilostazol
- Prasugrel
- Dipyridamole
They are used to prevent myocardial infarction, strokes, and clots in coronary arteries, especially in patients with known coronary artery disease or peripheral vascular disease.
How They Work:
They prevent platelets from sticking together, thereby reducing clot formation.
Side Effects:
- Bleeding and bruising
- GI upset (nausea, vomiting, heartburn)
- Rash and headache
- Note: Aspirin is not for pediatric patients because it can lead to Reye’s syndrome.
Monitoring:
- Monitor for bleeding by checking for a decrease in platelet count and hemoglobin/hematocrit levels.
- Assess for bleeding in urine, stool, gums, and check for stomach pain.
Angiotensin II Receptor Blockers (ARBs)
Next are the Angiotensin II Receptor Blockers (ARBs). These medications block angiotensin II receptors, preventing vasoconstriction and promoting vasodilation. Examples include
- Olmesartan
- Valsartan
- Losartan
- Telmisartan
- Candesartan
- Irbesartan (notice the “-sartan” ending).
Uses:
- Treat hypertension
- Manage diabetic nephropathy (protect kidney function)
- Reduce the workload on the heart in heart failure
- Assist in peripheral arterial disease
How They Work:
They block the activation of angiotensin II type 1 receptors, dilate blood vessels, and decrease aldosterone secretion, which helps excrete extra water and sodium while retaining potassium.
Side Effects:
- Dizziness and hypotension
- Increased potassium levels
- GI upset
- Rarely, angioedema (swelling of the face, lips, mouth, or throat)
Monitoring:
- Monitor potassium levels and renal function (BUN and creatinine).
- Assess blood pressure and watch for signs of hypotension.
Anti-Arrhythmics
The anti-arrhythmics work against abnormal heart rhythms. Medications in this class include:
- Flecainide
- Procainamide
- Amiodarone
- Quinidine
- Lidocaine
- Propafenone
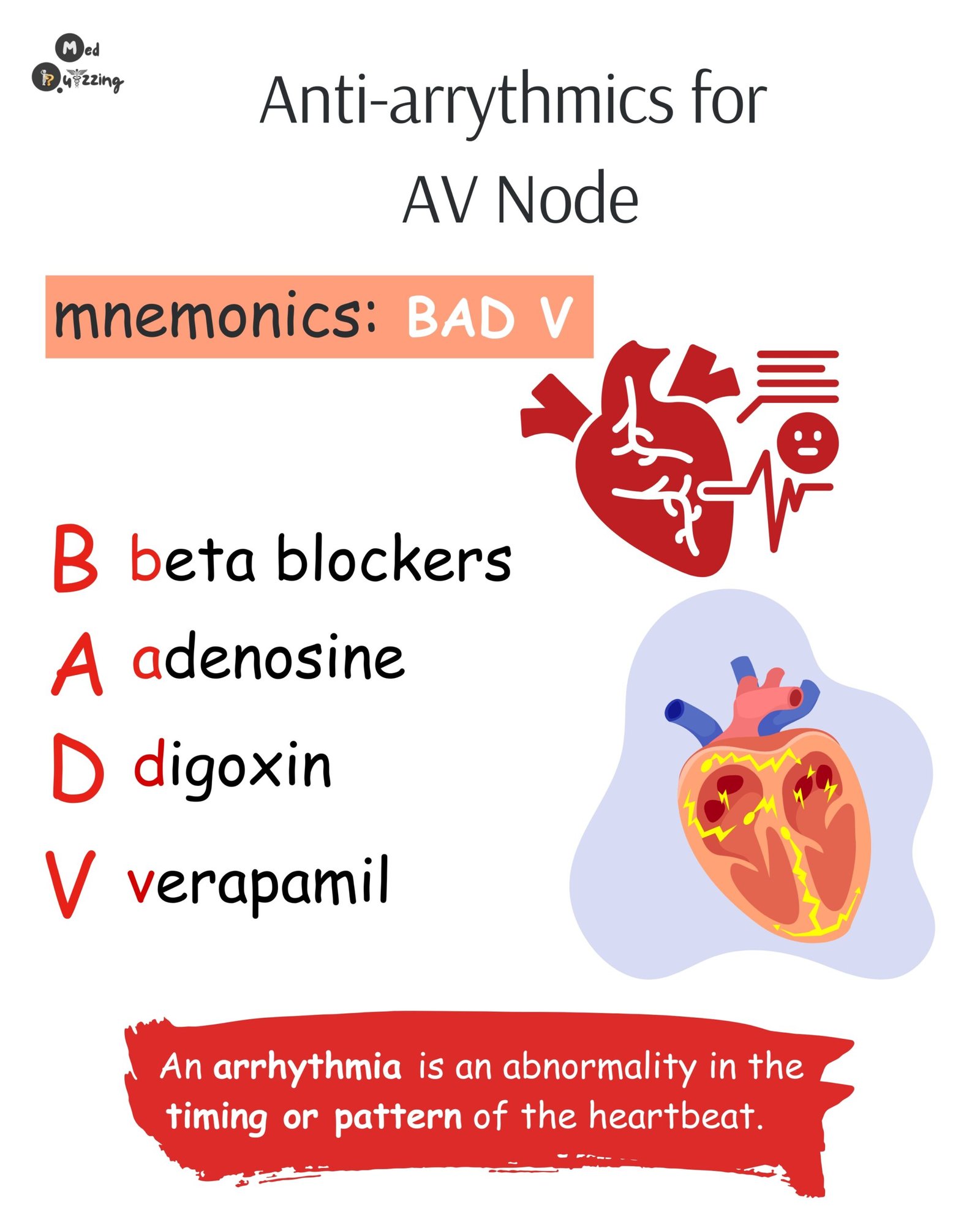
They are effective for treating fast arrhythmias such as atrial fibrillation, atrial flutter, ventricular tachycardia, and supraventricular tachycardia (SVT).
How They Work:
They slow down the electrical activity in the heart by altering various ion channels, which helps slow down a fast heart rate. However, this slowing can sometimes be excessive, leading to side effects such as:
- Bradycardia and hypotension
- Development of a new arrhythmia
- Heart block (prolonged PR interval)
- QT interval prolongation (which can lead to torsades de pointes)
- Altered potassium and magnesium levels
- With amiodarone, potential lung toxicity and skin rash
Monitoring:
- Monitor heart rhythm (ECG), blood pressure, and electrolyte levels.
- Be cautious with IV administration, as some protocols (e.g., for amiodarone) require central line administration and chest x-rays due to the risk of phlebitis.
Angiotensin Converting Enzyme (ACE) Inhibitors
ACE inhibitors are similar to ARBs but work by inhibiting the conversion of angiotensin I to angiotensin II. Medications
- Captopril
- Lisinopril
- Ramipril
- Quinapril
- Benazepril
(note the “-pril” ending).
Uses:
- Heart failure
- Hypertension
- Post-myocardial infarction management
- Protection of renal function in diabetic nephropathy
How They Work:
They inhibit the renin-angiotensin-aldosterone system (RAS), preventing vasoconstriction and promoting vasodilation.
Side Effects:
- A persistent dry cough (due to increased bradykinin)
- Dizziness
- Increased potassium levels
- Angioedema
Monitoring:
- Monitor potassium levels and renal function (BUN and creatinine).
- Assess for the development of a persistent cough and signs of angioedema.
Beta Blockers
Beta blockers block beta receptors in the body, reducing the effects of norepinephrine and epinephrine. Medications include atenolol
- Esmolol
- Metoprolol
- Propranolol
- Sotalol
- Timolol
(note the “-olol” ending).
Uses:
- Hypertension
- Stable angina
- Certain arrhythmias
- Heart failure
- Migraines, glaucoma, and tremors
How They Work:
By blocking beta receptors, these medications help “chill out” the sympathetic nervous system, reducing heart rate and blood pressure.
Side Effects:
- Excessive slowing of the heart (bradycardia)
- Heart block (2nd or 3rd degree)
- Exacerbation of heart failure
- Worsening of asthma or COPD (especially with non-selective beta blockers)
- Orthostatic hypotension
Monitoring:
- Monitor ECG, heart rate, and blood pressure.
- Watch for signs of heart failure exacerbation (e.g., jugular venous distension, weight gain, swelling, or difficulty breathing).
- Educate patients on the importance of tapering off beta blockers rather than quitting abruptly.
- For diabetic patients, note that beta blockers can mask signs of hypoglycemia.
Calcium Channel Blockers
Calcium channel blockers inhibit L-type calcium channels, promoting vasodilation and vessel relaxation. Examples include
- Amlodipine
- Felodipine
- Nifedipine
- Verapamil
- Diltiazem
(notice some generic names end in “-dipine”).
Uses:
- Hypertension
- Angina
- SVT, atrial fibrillation
- Migraines
How They Work:
They block calcium channels, leading to vasodilation. This effect can cause side effects such as:
- Bradycardia
- Hypotension
- Reflex tachycardia
- First-degree heart block
- GI problems like constipation
- Gingival hyperplasia
Monitoring:
- Monitor heart rate, blood pressure, and ECG.
- Advise patients to avoid grapefruit juice, which can affect medication efficacy.
- Educate patients about dietary fiber and oral hygiene to combat constipation and gingival hyperplasia.
- Instruct patients to change positions slowly to prevent orthostatic hypotension.
Cardiac Glycosides
Cardiac glycosides (e.g., digoxin) are used to treat heart failure, cardiogenic shock, atrial fibrillation, or atrial flutter.
- Digoxin
How They Work:
They exhibit three main effects:
- Positive inotropic effect: Increases the force of cardiac contractions.
- Negative chronotropic effect: Slows down the heart rate.
- Negative dromotropic effect: Slows down electrical conduction through the AV node.
These effects make the heart stronger, slower, and more controlled.
Side Effects & Toxicity:
- Early signs of toxicity include nausea and vomiting.
- Later, patients may experience vision changes (yellowish-green halos) and ECG changes (arrhythmias).
- Electrolyte imbalances (especially low potassium, low magnesium, or high calcium) increase the risk of digoxin toxicity, as do elderly patients or those on calcium channel blockers.
Monitoring:
- Measure the apical pulse before administering each dose.
- Follow hospital protocols (e.g., holding the dose if the apical pulse is less than 60 in adults, less than 70 in children, and less than 90–100 in infants).
- Ensure patients maintain adequate potassium intake and monitor ECG and electrolyte levels.
Statins
Statins are essential for treating high cholesterol. Medications in this class include
- Simvastatin
- Lovastatin
- Pravastatin
- Rosuvastatin
- Atorvastatin
(note the “-statin” ending).
Uses:
They help lower LDL (bad cholesterol), increase HDL (good cholesterol), reduce triglyceride levels, and stabilize fatty plaques in the heart, thus preventing myocardial infarction.
How They Work:
They inhibit HMG-CoA reductase, blocking the conversion of mevalonic acid and thereby reducing cholesterol synthesis.
Side Effects:
- Sore muscles (with the risk of progressing to statin-induced rhabdomyolysis)
- Increased liver enzymes
- GI upset
- Elevated glucose levels in type 2 diabetes
Monitoring:
- Monitor for signs of rhabdomyolysis (e.g., increased creatinine kinase, dark urine, and kidney damage).
- Advise patients to avoid grapefruit juice to prevent increased toxicity.
- Check liver enzymes (ALT, AST) regularly.
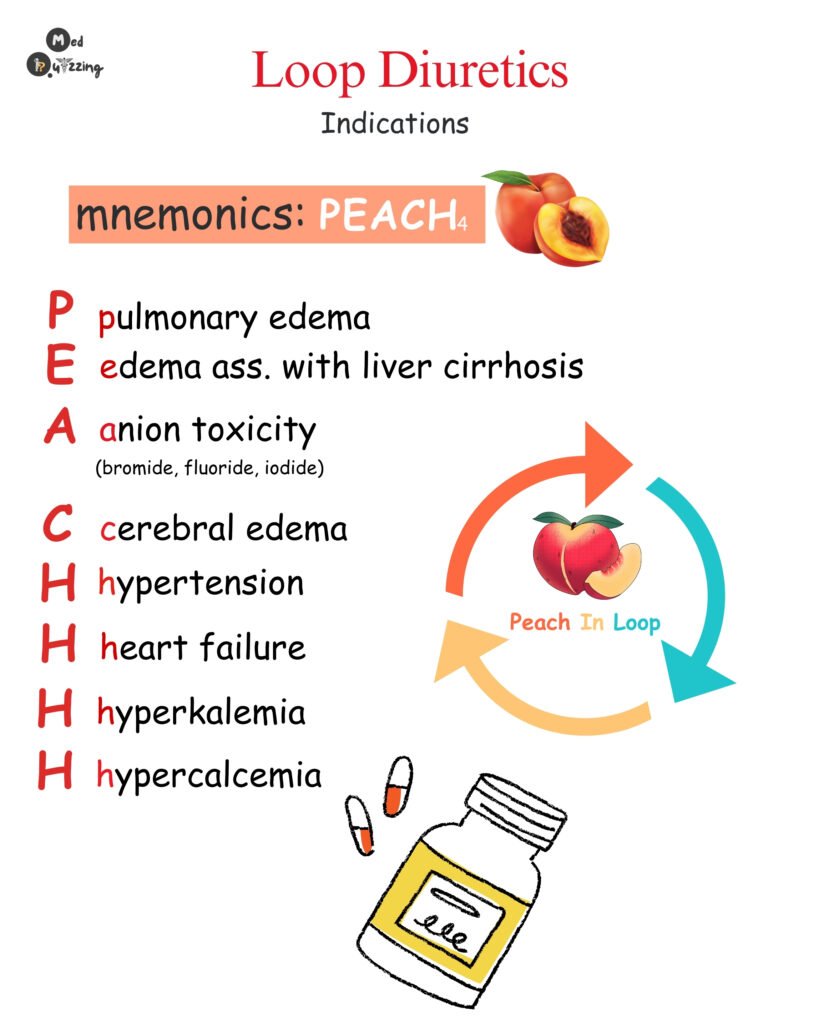
Diuretics
Diuretics aim to increase urination to rid the body of extra fluid. There are four main groups:
Loops:
- Furosemide
- Torsemide
Thiazides:
- HCTZ
- Chlorthalidone
K + sparing:
- Spironolactone,
- Amiloride
Carbonic anhvdrase inhibitors:
- Acetazolamide
Uses:
They are used to treat fluid overload (as seen in heart failure), hypertension, electrolyte disturbances, and even glaucoma (with carbonic anhydrase inhibitors).
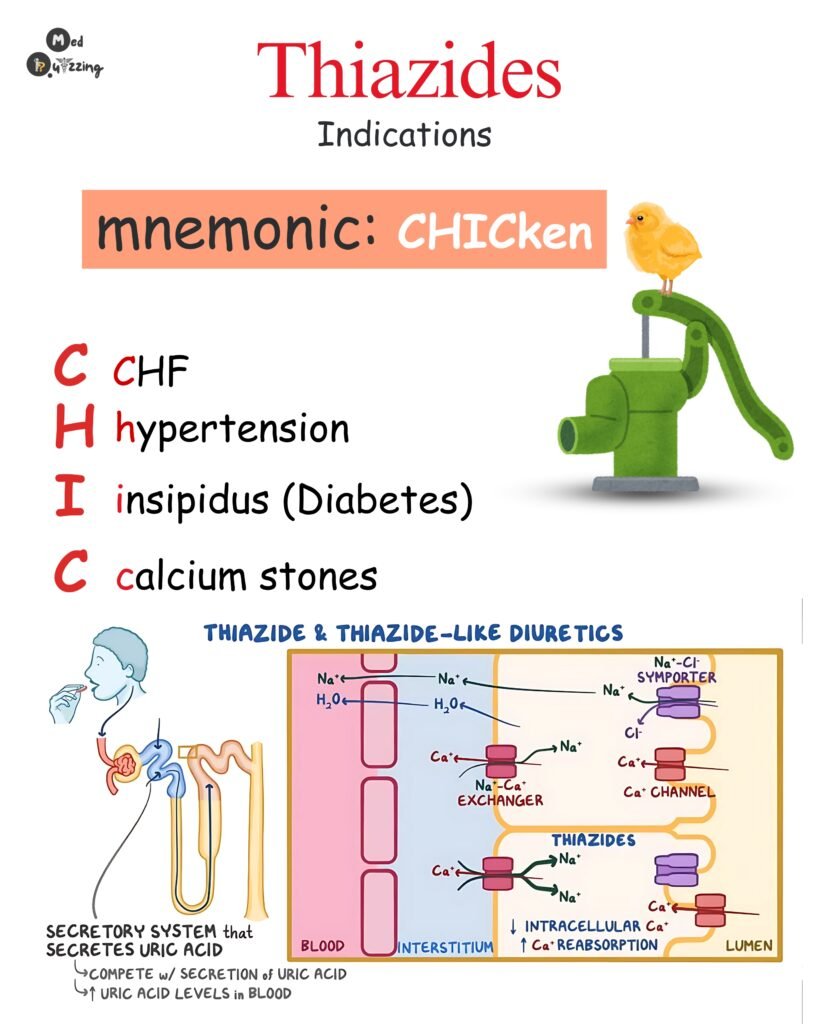
How They Work:
They act on specific parts of the nephron (e.g., loop diuretics work on the Loop of Henle) to remove excess fluid.
Side Effects:
- Electrolyte imbalances (loops and thiazides can drop potassium and sodium levels; potassium-sparing diuretics can increase potassium)
- Dehydration and potential renal impairment
- Loop diuretics may cause ototoxicity (affecting hearing), while thiazides may cause photosensitivity.
Monitoring:
- Monitor fluid status (intake and output, daily weights) and electrolyte levels (potassium, sodium).
- Check renal function (BUN and creatinine) and blood pressure.
- Assess lung sounds in patients with heart failure.
- Monitor hearing, especially in patients on loop diuretics.
Vasodilators
Vasodilators work by opening up blood vessels to improve blood flow. Examples include nitroglycerin
- Minoxidil
- Hydralazine
- Isosorbide
- Mononitrate
Uses:
They are useful in treating angina (by dilating narrowed coronary arteries), heart failure (reducing the heart’s workload), hypertension, coronary artery disease, pulmonary hypertension, and peripheral vascular disease.
How They Work:
By dilating blood vessels, they decrease overall blood pressure, which reduces the workload on the heart.
Side Effects:
- Hypotension
- Flushing (common with sublingual nitroglycerin)
- Headaches
- Orthostatic hypotension
- Nausea, vomiting, reflex tachycardia, and edema
Monitoring:
- Monitor blood pressure, heart rate, and ECG.
- Assess the patient’s response, particularly chest pain, and note any changes in the pain’s onset, location, quality, or frequency.
- Educate patients to change positions slowly to prevent fainting.
Angiotensin Receptor Nepril Inhibitors (ARNIs)
Lastly, we have Angiotensin Receptor Nepril Inhibitors (ARNIs), a combination drug class that includes components such as
- Sacubitril/Valsartan (brand name: Entresto).
They are used to treat heart failure with reduced ejection fraction.
How They Work:
They inhibit angiotensin II and neprilysin, preventing the breakdown of natriuretic peptides (ANP and BNP). This results in vasodilation and diuresis, which are beneficial for heart failure management.
Side Effects:
- Hypotension
- High potassium levels
- Angioedema
- Renal insufficiency
- Cough and dizziness
Monitoring:
- Do not administer this medication with an ACE inhibitor for at least 36 hours before or after the ACE inhibitor is given.
- Monitor electrolytes and renal function (BUN, creatinine), blood pressure, and heart rate.
- Assess intake and output and daily weights.
- Evaluate for worsening heart failure symptoms (e.g., crackles, productive cough, chest pain, weight gain, or difficulty breathing).