What is Angina Pectoris? Symptoms, Causes
What is Angina Pectoris?
Angina pectoris, commonly referred to as angina, is a condition characterized by chest pain resulting from an inadequate supply of oxygen to the heart muscle. This pain is often severe, crushing, and accompanied by a sensation of pressure and suffocation, typically felt just behind the breastbone. While angina itself is a significant health concern, it can also act as a warning sign or precursor to a heart attack, making early recognition and management critical.
The most common cause of angina is a blockage or narrowing in the coronary arteries—vital blood vessels that supply oxygen-rich blood to the heart. These blockages often result from plaque buildup within the arteries, a condition known as atherosclerosis. During physical exertion, when the heart demands more oxygen, this narrowing can become symptomatic, leading to angina.
However, other causes, such as inflammation, infection, or injury to the coronary arteries, can also contribute to this condition. Several factors increase the risk of developing angina, including chronic conditions such as diabetes, high blood pressure, and high cholesterol. Lifestyle choices such as smoking, physical inactivity, and poor dietary habits further compound the risk, as do obesity, stress, and advancing age.
Etiology of Angina Pectoris
Angina pectoris occurs when the heart receives insufficient blood supply through the coronary arteries, leading to a mismatch between oxygen demand and supply. The etiology can be categorized into common causes, mechanisms, and specific types based on their underlying triggers.
Primary Etiological Factors
- Atherosclerosis (Most Common Cause)
- Gradual buildup of plaque within the coronary arteries reduces blood flow.
- Leads to progressive narrowing or occlusion of the vessel lumen, restricting oxygen supply to the myocardium.
- Vasospasm
- Transient narrowing of coronary arteries caused by spasms in the arterial wall.
- Responsible for a specific type of angina known as Prinzmetal (variant) angina.
- Ruptured Plaque and Vasoconstriction
- Sudden rupture of atherosclerotic plaque, coupled with vasoconstriction, can temporarily block coronary arteries.
- Commonly associated with unstable angina.
Pathophysiology of Angina
Angina, or chest pain, arises from the inability of the coronary arteries to deliver adequate oxygenated blood to the myocardium. This condition typically results from a mismatch between myocardial oxygen demand and supply due to impaired blood flow through the coronary arteries.
1. Coronary Artery Blood Supply
The coronary arteries originate from the aorta and supply oxygen-rich blood to the myocardium. There are two main coronary arteries:
- Left Coronary Artery (LCA): Supplies the left atrium, left ventricle, and the interventricular septum through its branches:
- Left Anterior Descending (LAD) artery.
- Left Circumflex (LCx) artery.
- Right Coronary Artery (RCA): Supplies the right atrium, right ventricle, parts of the left ventricle, and the sinoatrial (SA) and atrioventricular (AV) nodes through its branches:
- Right Marginal Artery.
- Right Posterior Descending Artery (PDA).
These arteries act as a vascular network, delivering blood to meet the high metabolic demands of the myocardium.
2. Mechanism of Ischemia and Angina
Ischemia refers to reduced blood flow and oxygen supply to tissues. In angina, ischemia occurs due to partial or transient obstruction of coronary blood flow. The causes of ischemia include:
- Atherosclerosis: The most common cause. Atherosclerotic plaques reduce the lumen of coronary arteries, limiting blood flow.
- Vasospasm: Transient constriction of coronary arteries can cause ischemia without significant plaque buildup (as seen in variant angina).
When coronary artery obstruction exceeds 70%, blood flow becomes insufficient to meet myocardial demands during exertion. At >90% obstruction, ischemia may occur even at rest.
Pathological sequence:
- Decreased coronary blood flow → reduced oxygen delivery to myocardial cells.
- Cellular hypoxia → anaerobic metabolism and lactic acid accumulation.
- Lactic acid and metabolic byproducts stimulate nerve endings, causing chest pain (angina).
3. Types of Angina
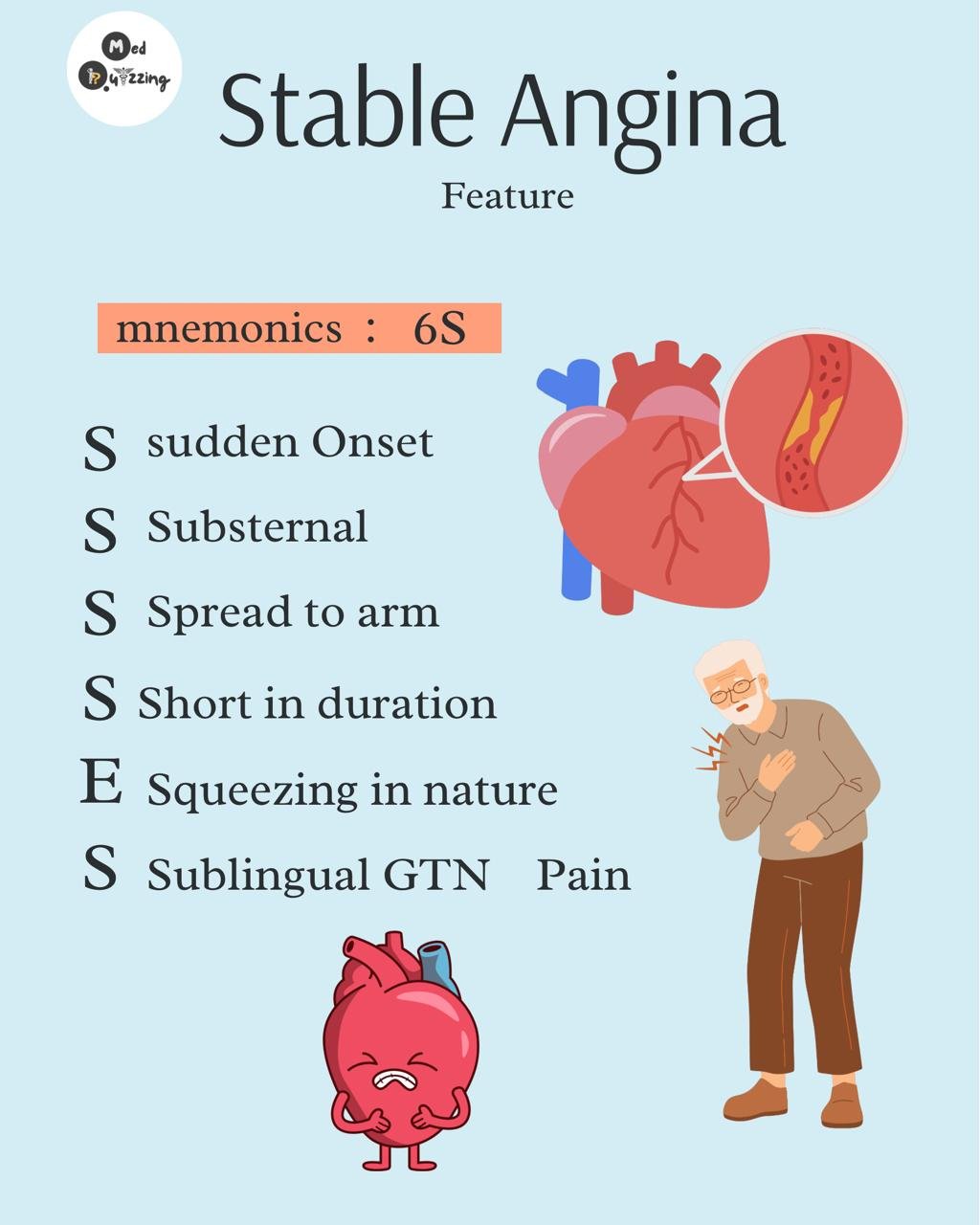
- Stable Angina:
- Caused by fixed atherosclerotic plaque.
- Pain occurs during exertion or stress when oxygen demand exceeds supply.
- Unstable Angina:
- Caused by plaque rupture, thrombosis, or progressive atherosclerosis.
- Pain occurs at rest or with minimal exertion, often more severe and unpredictable.
- Variant (Prinzmetal) Angina:
- Caused by transient coronary artery spasm.
- Occurs at rest and is not related to physical exertion.
4. Myocardial Impact of Ischemia
- Left Coronary Artery Blockage: Leads to ischemia of the left ventricle, impairing its pumping ability and reducing cardiac output. Severe ischemia may progress to myocardial infarction.
- Right Coronary Artery Blockage: Can affect electrical conduction by ischemia of the SA or AV nodes, leading to arrhythmias.
In prolonged ischemia, necrosis of myocardial tissue develops, causing irreversible damage.
Signs and Symptoms of Angina Pectoris

Angina pectoris presents with distinct and sometimes atypical symptoms due to reduced blood flow to the heart muscle. The hallmark symptom is chest pain or discomfort, but the presentation can vary depending on the severity and type of angina. Below is a detailed outline of its signs and symptoms:
Typical Symptoms
- Chest Pain or Discomfort
- Described as a pressure, heaviness, or fullness in the center of the chest.
- Often likened to a “vise squeezing the chest” or a heavy weight resting on it.
- Pain duration typically ranges from a few minutes to 15 minutes, especially during physical exertion or emotional stress.
- Radiation of Pain
- Pain may radiate to the neck, jaw, shoulders, or arms (commonly the left arm).
- Occasionally, pain may extend to the back or upper abdomen.
- Shortness of Breath (Dyspnea)
- Occurs due to inadequate oxygenation of the myocardium, leading to difficulty breathing.
- Nausea and Vomiting
- Result from the activation of the vagus nerve during ischemic episodes.
- Profuse Sweating (Diaphoresis)
- Sweating is triggered by the sympathetic nervous system as a response to chest pain or discomfort.
- Fatigue
- Generalized weakness, particularly during exertion, is a common associated symptom.
- Dizziness or Lightheadedness
- Results from reduced cardiac output and subsequent insufficient blood supply to the brain.
- Anxiety or Sense of Impending Doom
- A common psychological symptom, likely linked to autonomic responses and the distress of chest pain.
Atypical Symptoms
Angina can present with less characteristic features, especially in certain populations such as women, diabetics, and the elderly:
- Indigestion or Heartburn-like Discomfort
- Nausea or Epigastric Pain resembling gastrointestinal upset.
- Vomiting associated with ischemic episodes.
Key Features of Different Types of Angina
- Stable Angina:
- Chest pain or discomfort occurs predictably during physical activity or stress.
- Symptoms are relieved by rest or nitroglycerin.
- Unstable Angina:
- Chest pain is sudden, severe, and can occur at rest.
- Often more prolonged and not relieved by rest or standard medications.
- Variant (Prinzmetal) Angina:
- Episodes of chest pain occur at rest, often in the early hours of the morning.
- Pain is due to coronary vasospasm rather than exertion.
Stages of Angina Pectoris
Angina is clinically classified into five stages based on symptom severity and functional limitations, as outlined by the Canadian Cardiovascular Society (CCS). This classification helps in understanding the progression of the disease and guiding appropriate management.
Stage 0: Silent Ischemia
- Description:
- The mildest form of angina where the patient is asymptomatic.
- Despite the lack of symptoms, the heart muscle remains underperfused (reduced blood flow).
- Key Feature:
- No noticeable chest pain or discomfort.
Stage 1: Symptoms with Strenuous Activity
- Description:
- Symptoms (e.g., chest pain or discomfort) occur only during intense physical exertion.
- The patient can carry out normal daily activities without limitations.
- Key Feature:
- Pain or discomfort during heavy exercise or physical stress.
Stage 2: Symptoms with Normal Physical Activities
- Description:
- Chest pain or discomfort occurs during ordinary activities, such as walking or climbing stairs.
- The patient begins to avoid moderate physical activities to prevent symptoms.
- Key Feature:
- Angina symptoms are triggered by routine exertion.
Stage 3: Symptoms with Daily Activities
- Description:
- Symptoms become more frequent and occur during minimal daily activities, such as walking short distances or light household tasks.
- Increased avoidance of daily activities due to discomfort.
- Key Feature:
- Severe limitations in daily functioning due to angina.
Stage 4: Symptoms at Rest (Unstable Angina)
- Description:
- The most severe stage of angina.
- Chest pain or discomfort occurs even at rest or during minimal exertion.
- Represents unstable angina, which carries a higher risk of progression to myocardial infarction.
- Key Feature:
- Persistent and unpredictable symptoms at rest, indicating critical ischemia.
Diagnosis of Angina Pectoris
The diagnosis of angina pectoris involves assessing symptoms, conducting physical examinations, and performing various tests to confirm the underlying cardiac issue. The following methods are commonly used:
Electrocardiogram (ECG)
This test evaluates the heart’s electrical activity and helps identify ischemic changes. In cases of angina, the ECG may show abnormalities such as ST-segment elevation (indicating myocardial infarction) or depression, which points to ischemia. A normal ECG could still warrant further testing if symptoms suggest cardiac involvement.
Stress Testing
A stress test measures how the heart performs under physical exertion. Patients are monitored for changes in heart rhythm, blood pressure, and ECG readings while walking on a treadmill or cycling. This helps reveal ischemic changes not evident at rest.
Echocardiogram
Using sound waves, this test provides a detailed image of the heart’s structure and function. It can identify areas of the heart that are not receiving adequate blood flow or have been damaged due to ischemia.
Nuclear Stress Test
This advanced test uses a radioactive substance to evaluate blood flow to the heart during rest and exertion. It highlights areas with reduced perfusion and provides a more detailed assessment than a traditional stress test.
Cardiac Markers
Blood tests detect enzymes like troponin and CK-MB, which are released during myocardial damage.
- Troponin: The most specific marker, elevated within 6 hours of an infarction and remains high for up to 2 weeks.
- CK-MB: Useful for identifying reinfarctions as it normalizes within 48–72 hours.
Imaging Studies
- Chest X-Ray: Helps rule out other conditions like pulmonary causes of chest pain (e.g., pneumonia or pleural effusion).
- Coronary Angiography: Visualizes coronary arteries using X-ray imaging to identify blockages or narrowed vessels.
- Cardiac CT or MRI: Provides detailed images of the heart and blood vessels, revealing structural abnormalities or ischemic areas.
Differential diagnosis of angina pectoris
If no significant findings are evident from cardiac tests, other potential causes of chest pain, such as pulmonary or gastrointestinal disorders, must be explored.
Treatment of Angina Pectoris
The management of angina pectoris focuses on relieving symptoms, improving quality of life, and preventing complications such as myocardial infarction. Treatment strategies include lifestyle modifications, medications, and interventional procedures.
Lifestyle Modifications
Lifestyle changes form the foundation of angina management. These include:
- Smoking cessation: Reduces cardiovascular risk.
- Healthy diet: Emphasizes fruits, vegetables, and whole grains while minimizing saturated fats.
- Regular exercise: Improves cardiovascular fitness and reduces ischemic symptoms.
- Weight management: Helps control blood pressure, cholesterol, and diabetes.
However, lifestyle changes alone may not suffice for many patients, necessitating medications or procedures.
Medications
- Nitrates
- Relax vascular smooth muscles, dilate veins and coronary arteries, and reduce myocardial oxygen demand.
- Sublingual nitroglycerin: Provides immediate relief during acute angina episodes.
- Long-acting nitrates like isosorbide mononitrate help prevent attacks.
- Side effects include headaches, flushing, and hypotension.
- Beta Blockers
- Decrease heart rate, contractility, and myocardial oxygen demand.
- Examples: Metoprolol and Atenolol (selective beta-1 blockers).
- Benefits include reduced frequency and severity of attacks, improved exercise tolerance, and decreased risk of myocardial infarction and death.
- Avoid non-selective beta blockers in asthma or severe bradycardia.
- Calcium Channel Blockers (CCBs)
- Two subtypes:
- Dihydropyridines (e.g., Amlodipine): Cause vasodilation and relieve coronary artery spasm.
- Non-dihydropyridines (e.g., Verapamil, Diltiazem): Slow AV conduction, reduce heart rate, and decrease myocardial oxygen demand.
- Useful for variant angina and patients intolerant to beta blockers. Avoid in severe heart failure.
- Two subtypes:
- Antiplatelet Drugs
- Aspirin: Prevents clot formation by inhibiting platelet aggregation.
- Clopidogrel: Used in patients intolerant to aspirin.
- Statins
- Lower cholesterol levels and stabilize atherosclerotic plaques.
- Ranolazine
- Sodium channel blocker that reduces myocardial calcium overload and improves diastolic function.
- Indicated for chronic angina.
- Antihypertensive Medications
- Lower blood pressure to reduce cardiac workload.
Interventional Procedures
- Percutaneous Coronary Intervention (PCI)
- A minimally invasive procedure where a balloon is used to widen narrowed arteries, often followed by stent placement to keep the artery open.
- Effective in relieving symptoms and improving blood flow.
- Coronary Artery Bypass Grafting (CABG)
- Surgical bypass of blocked coronary arteries using a graft from another part of the body.
- Recommended for patients with severe or multiple arterial blockages.
Prognosis of Angina Pectoris
The prognosis of angina pectoris depends on the severity and underlying cause of the condition. With proper management, including medications and lifestyle changes, many patients can experience a significant reduction in symptoms and improved quality of life.
However, untreated or poorly managed angina can lead to an increased risk of heart attacks, heart failure, and other cardiovascular complications. Early intervention is key to improving long-term outcomes.


great work
Informative