What is Human Metapneumovirus (HMPV)?? Symptoms, Causes
What is Human Metapneumovirus (HMPV)??
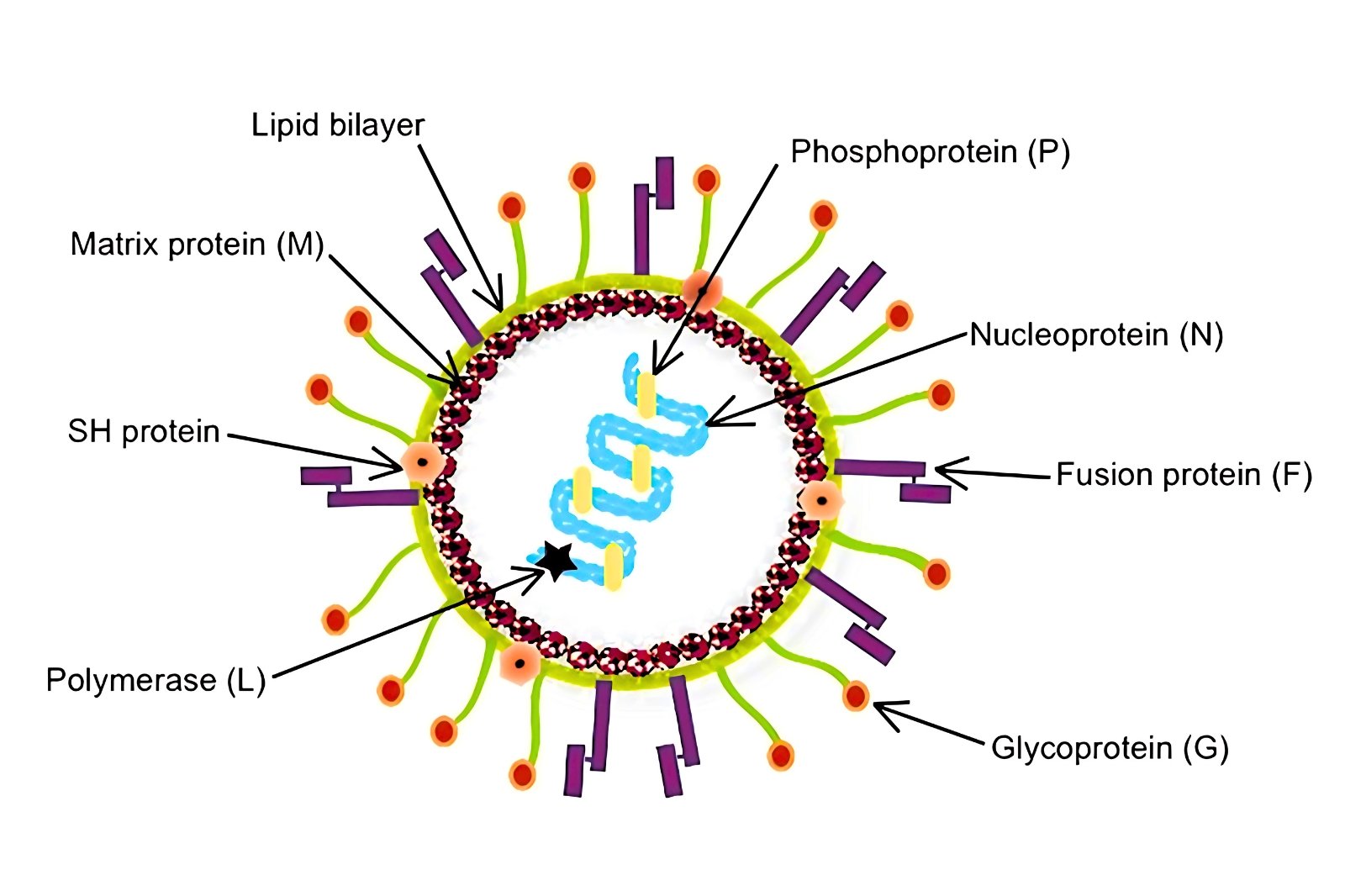
Human metapneumovirus (HMPV) is not a newly discovered virus; it has been responsible for infections for over six decades. First identified in 2001 in the Netherlands, the virus was found to predominantly impact children. HMPV is a large, enveloped, negative-sense RNA virus belonging to the Pneumoviridae family.
In 2016, it underwent reclassification and was designated as a metapneumovirus, distinguishing it from the orthopneumovirus family, which includes the respiratory syncytial virus (RSV). Despite its long history of causing infections, HMPV remains a significant pathogen, particularly in pediatric populations.
Subtypes of HMPV:
Human metapneumovirus (HMPV) is classified into two primary subtypes:
- HMPV-A
- HMPV-B
These subtypes are further divided into four distinct genetic lineages:
- A1
- A2
- B1
- B2
Although the genetic variations between these lineages are relatively minor, all of them are capable of causing illness. During outbreaks or seasonal peaks, one strain often emerges as the dominant variant, influencing the spread and impact of the virus during that period. Despite their subtle differences, all subtypes and lineages remain significant contributors to HMPV-related infections.
Pathogenesis:
Human metapneumovirus (HMPV) is a respiratory virus that specifically targets the respiratory system. It infects the body by binding to integrin alpha-5 beta-1, a receptor that plays a key role in facilitating the virus’s entry into epithelial cells within the respiratory tract.
Once the virus establishes infection, it triggers mucus hyperproduction and causes hyperplasia, or excessive growth, of the respiratory epithelium. These changes lead to airway obstruction and heightened airway responsiveness, which can significantly worsen respiratory conditions such as asthma. As a result, HMPV not only causes acute respiratory symptoms but also has the potential to exacerbate pre-existing respiratory disorders.
Transmission:
Human metapneumovirus (HMPV) is transmitted from person to person primarily through respiratory droplets, aerosols, and contact with contaminated surfaces (fomites), though it is not typically spread through small aerosols. Maintaining a distance of at least six feet from infected individuals can significantly lower the risk of contracting the virus.
In healthcare settings, nosocomial infections, or hospital-acquired infections, are a concern, particularly when healthcare workers or attendants are unaware of their infection status. To mitigate the spread of HMPV in such environments, isolating or cohorting patients in private rooms or designated areas can be an effective strategy. These measures help reduce the risk of transmission and protect vulnerable populations within healthcare facilities.
Incubation Period:
The incubation period for human metapneumovirus (HMPV) ranges from 5 to 7 days, a period during which viral shedding reaches its peak. Symptoms of the infection usually appear after this incubation phase and tend to resolve within 3 to 5 days after they begin.
As a result, HMPV is generally considered a self-limiting disease, meaning it typically runs its course without the need for extensive medical intervention. However, the severity and duration of symptoms can vary depending on the individual’s age, immune status, and underlying health conditions.
Epidemiology:
Human metapneumovirus (HMPV) is a globally widespread virus, with cases reported in numerous countries, including the Netherlands, the United Kingdom, Finland, Australia, Canada, Kenya, China, and Norway. In 2018 alone, there were an estimated 14.2 million cases of HMPV in children under the age of five, highlighting its significant impact on this vulnerable population.
While the virus can affect individuals of all age groups, it tends to be particularly severe in children under five, older adults, and those with chronic health conditions, such as chronic obstructive pulmonary disease (COPD), transplant recipients, or immunocompromised patients. These high-risk groups are more likely to experience severe symptoms and complications, underscoring the importance of monitoring and managing HMPV infections in susceptible populations.
Seasonal Variation:
- In Western countries like the United States, HMPV outbreaks occur in late winter and early spring.
- In regions like Hong Kong and China, outbreaks are more common in late spring and summer.
Cross-Reactivity with RSV:
- There is partial immunity between HMPV and RSV, meaning prior infection with RSV may offer some protection against HMPV.
Symptoms:
- In Children: Symptoms include cough, rhinitis, fever, and wheezing. Wheezing is often disproportionate compared to other viral infections.
- In Adults: Symptoms include cough, nasal congestion, rhinitis, hoarseness, and persistent wheezing. Wheezing may continue even after other symptoms resolve.
- HMPV can cause upper and lower respiratory infections, bronchitis, severe pneumonia, and, in rare cases, acute respiratory distress syndrome (ARDS) or encephalitis.
Risk Factors:
- Children: Premature birth, female sex, and specific genotypes (B1, B2) increase susceptibility.
- Adults: Recurrent infections are common, as most adults were likely exposed during childhood.
- Immunocompromised Individuals: Transplant recipients, HIV patients, and those with hematologic malignancies or lung transplants are at higher risk.
Diagnosis:
The diagnosis of human metapneumovirus (HMPV) relies on several laboratory techniques, with reverse transcription-polymerase chain reaction (RT-PCR) being the standard diagnostic tool. This method, similar to the testing used for COVID-19, detects the virus’s genetic material with high accuracy.
Multiplex PCR is another valuable technique, as it can identify multiple respiratory viruses, including HMPV, in a single test, making it efficient for diagnosing co-infections.
Serology and viral cultures are also available, they are primarily utilized for research purposes rather than routine clinical diagnosis. These diagnostic methods play a critical role in accurately identifying HMPV infections, enabling timely and appropriate patient management.
Treatment:
- There is no specific antiviral treatment for HMPV.
- Management is supportive, focusing on symptom relief (e.g., fever reducers, hydration, and respiratory support).
Prevention:
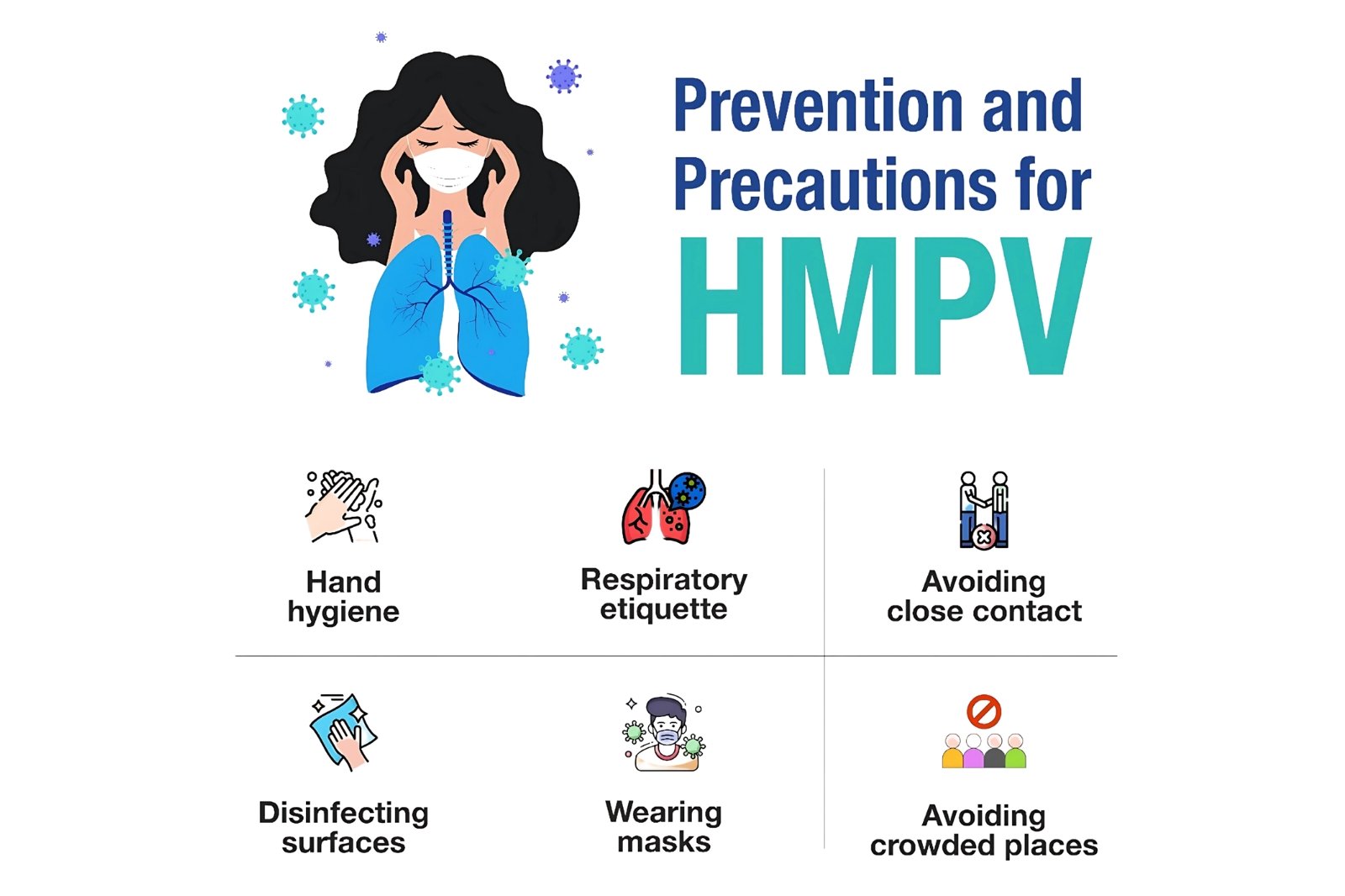
- Practice good hygiene, including handwashing and wearing masks.
- Maintain physical distance from infected individuals.
- In households with infected children, elderly or immunocompromised individuals should avoid close contact for 8 to 10 days.
- No vaccine is currently available.