Peripheral Vascular Disease (PVD) Peripheral Arterial (PAD) Venous Disease
What is PVD?
PVD is the impediment of the blood flow within the peripheral vascular system due to damage to the vessels that make up that system.
Your peripheral vascular system provides circulation to your arms, hands, feet, and legs. This is circulation outside of the heart and brain. With peripheral vascular disease, the condition can affect either the arterial system—known as peripheral arterial disease (PA D)—or the venous system, which is called peripheral venous disease.
Most patients will show signs and symptoms in their lower extremities. However, the signs and symptoms are completely different between arterial and venous disease.
Arterial and Venous Systems
Let’s quickly review the arterial and venous systems to understand the differences.
The arterial system carries oxygenated blood from the heart to the extremities and organs. In illustrations, the arterial system is represented in red.
Your heart, with the assistance of the lungs, oxygenates the blood. The heart then pumps this oxygenated blood out with great force. You can feel this when you palpate your arteries in your arms and feet.
Without sufficient oxygen, ischemia occurs and tissue begins to die.
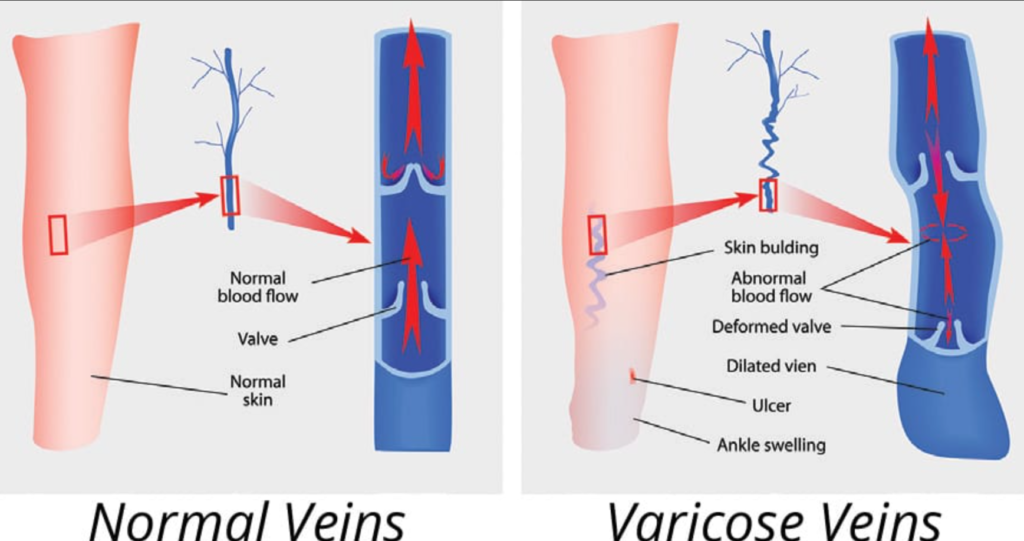
Conversely, the venous system carries deoxygenated blood from the extremities and organs back to the heart. In illustrations, this system is represented in blue.
The arterial system sends blood away from the heart, while the venous system returns it. This process works only if the veins and their valves are healthy.
Peripheral Arterial Disease (PA D)
Peripheral arterial disease occurs when fatty plaques accumulate in the arteries. This is known as atherosclerosis.
Atherosclerosis limits the amount of blood that reaches the extremities. When blood flow is reduced, patients experience pain.
The patient may develop arterial ulcers because the tissue is not being fed. If severe, tissue necrosis can occur, and the extremity may require amputation.

The Venous System and Peripheral Venous Disease
PVD affects the veins’ ability to return blood to the heart. When veins are damaged or their valves are overstretched, blood pools in the extremities. This results in venous congestion and pain.
Patients may experience heavy, throbbing pain and impaired tissue nutrition. Stagnant blood can break down the skin, causing brown pigmentation and venous stasis ulcers.
Cellulitis may also develop as a skin infection.
Risk Factors for PVD
Risk Factors for Peripheral Arterial Disease (PA D)
- Smoking/Tobacco Use: Causes constriction of the arteries.
- Uncontrolled Hypertension: High pressure damages the arteries.
- High Cholesterol/Obesity: Leads to atherosclerosis.
- Diabetes: Increases the risk of arterial damage.
Risk Factors for Peripheral Venous Disease
- Female Gender & Birth Control Use: Associated with increased risk.
- Pregnancy: Elevated venous pressure can damage veins.
- Obesity: Contributes to vein damage.
- Prolonged Sitting/Standing: Can overstretch the vein valves.
- Advanced Age: Increases the risk for venous issues.
Diving Deeper into PVD Types
Peripheral Arterial Disease (PA D)
In PA D, narrowing of the arteries results in reduced oxygenated blood reaching the extremities.
Ischemia occurs, and tissue integrity is compromised due to atherosclerosis. Fatty plaques may rupture, forming clots that further block blood flow.
Raynaud’s Disease
Raynaud’s disease is a type of arterial disease that involves vasospasm. It is triggered by cold or stress, causing fingers and toes to turn white, then blue, and finally red with tingling once the vasospasm subsides. Patients need to keep their extremities warm to prevent these episodes.

Buerger’s Disease
Buerger’s disease affects both arteries and veins. Inflammation and clot formation occur in the hands and feet. Smoking is a major risk factor, making smoking cessation essential.

Peripheral Venous Disease
Peripheral venous disease occurs when the veins cannot return blood efficiently to the heart.
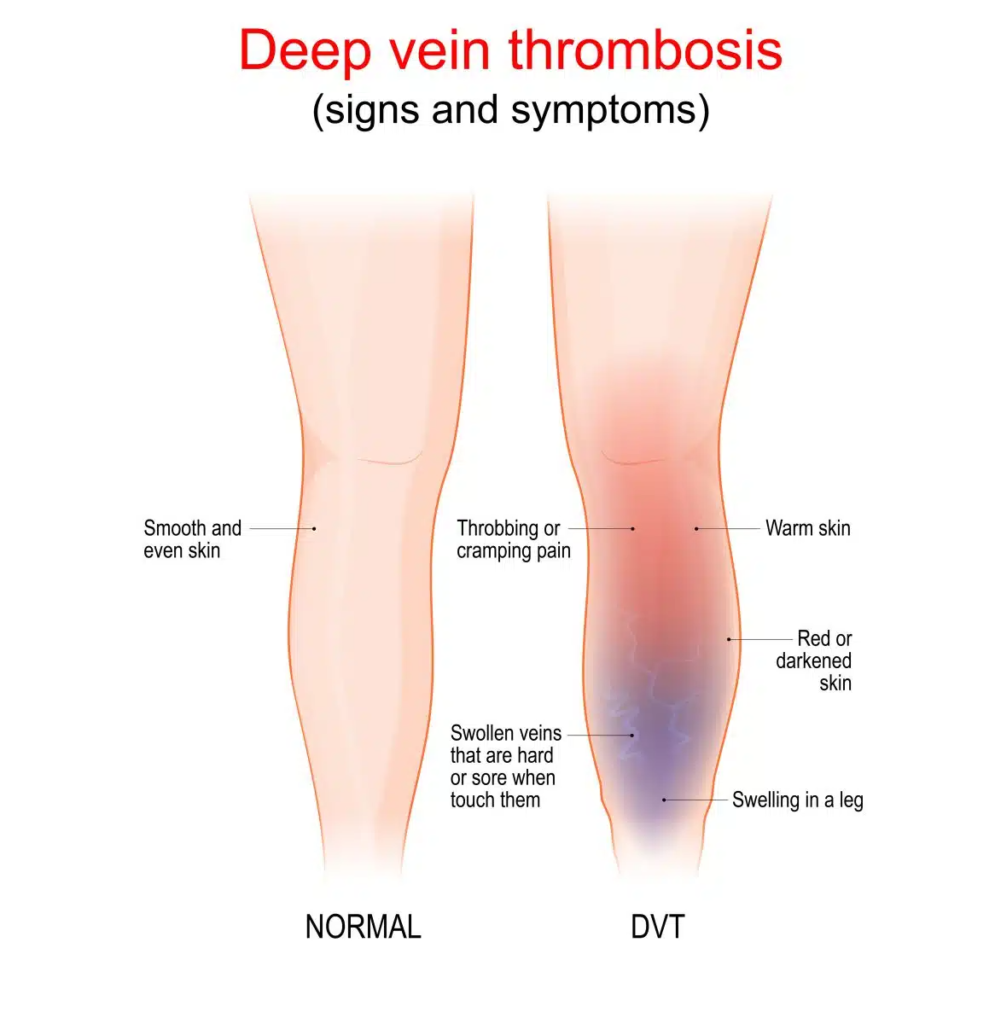
Conditions such as varicose veins, deep vein thrombosis (DVT), superficial venous thrombosis, and chronic venous insufficiency lead to pooling of blood and swelling.
DVT is dangerous because clots can travel to the lungs, causing a pulmonary embolism.
Differentiating Arterial and Venous Disease
Lower Extremity Positions
- Patients with arterial disease often report relief when they dangle their legs (dependent position) because it increases blood flow.
However, elevating the leg worsens pain due to further reduced blood flow. - In venous disease, elevating the legs helps reduce pain and swelling by assisting venous return, while dangling the legs worsens symptoms.
Pain Characteristics
- Arterial disease typically presents with sharp pain, worse at night (rest pain), and intermittent claudication during activity.
- Venous disease, on the other hand, is described as heavy, dull, throbbing, and achy, worsening with prolonged standing or sitting.
Skin Characteristics
In arterial disease, the skin is cool, thin, dry, and scaly with little hair. Dangling the leg may make the skin appear red and warm, while elevation makes it pale. In venous disease, the skin tends to be warm and thick, with brown pigmentation due to blood pooling.
Pulse Strength
- Arterial disease may result in weak or absent pulses, often detected with a Doppler.
- Venous disease usually shows normal pulses.
Edema
- Edema is uncommon in arterial disease. In venous disease, edema is common and often worsens by the end of the day.
Ulcer Characteristics
- Arterial ulcers are typically found on the toes, dorsum of the feet, or lateral ankle.
They have little drainage, a “punched out” appearance, and well-defined edges. - Venous ulcers usually occur on the medial lower leg, are swollen with significant drainage, and have irregular edges with granulation tissue.
Monitoring for PVD
For Peripheral Arterial Disease (PA D)
Monitor circulation by checking pulses frequently using a Doppler. Assess skin color, temperature, and sensation. Teach patients to avoid tight clothing or constrictive devices on their extremities. Advise patients to avoid extreme colds and to quit smoking.
Encourage adherence to medications, a low-fat diet, and a walking program to relieve intermittent claudication. Instruct patients to inspect their skin daily and test bathwater temperature to avoid burns.
For Peripheral Venous Disease
Focus on improving blood return by using compression stockings. Provide proper skin care and monitor for clots. Administer anticoagulants as prescribed. Educate patients on leg elevation to reduce edema and pain. Ensure proper wound care for venous stasis ulcers, possibly using zinc oxide wraps.