What is Pneumonia? Causes, symptoms, treatment
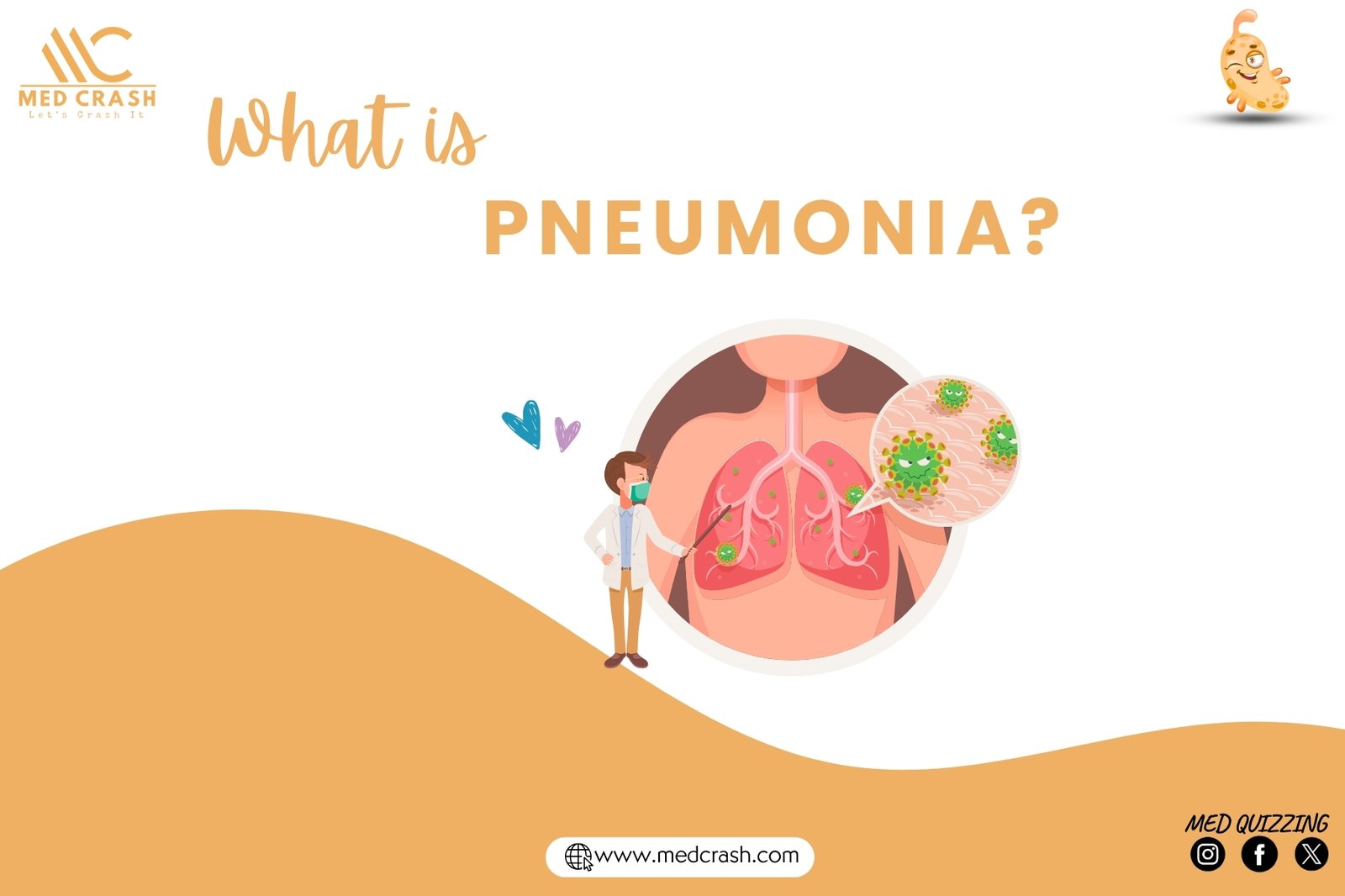
What is Pneumonia?
Pneumonia is a lower respiratory tract infection that causes inflammation of the alveoli (the tiny air sacs in the lungs responsible for gas exchange). When inflamed, these sacs fill with fluid, pus, or cellular debris, impairing oxygen exchange and leading to symptoms like hypoxemia (low blood oxygen) and respiratory acidosis.
Pathophysiology of Pneumonia
Normally, oxygen enters the lungs, travels through the bronchial tree, and reaches the alveoli, where it diffuses into the bloodstream. Carbon dioxide, a waste product, exits the bloodstream into the alveoli to be exhaled.
In pneumonia:
- Germs (bacteria, viruses, or fungi) invade the alveoli.
- The immune system responds by sending white blood cells, causing inflammation.
- Fluid and inflammatory cells accumulate in the alveoli, preventing proper gas exchange.
- Hypoxemia (low oxygen) and hypercapnia (high carbon dioxide) develop, leading to respiratory acidosis.
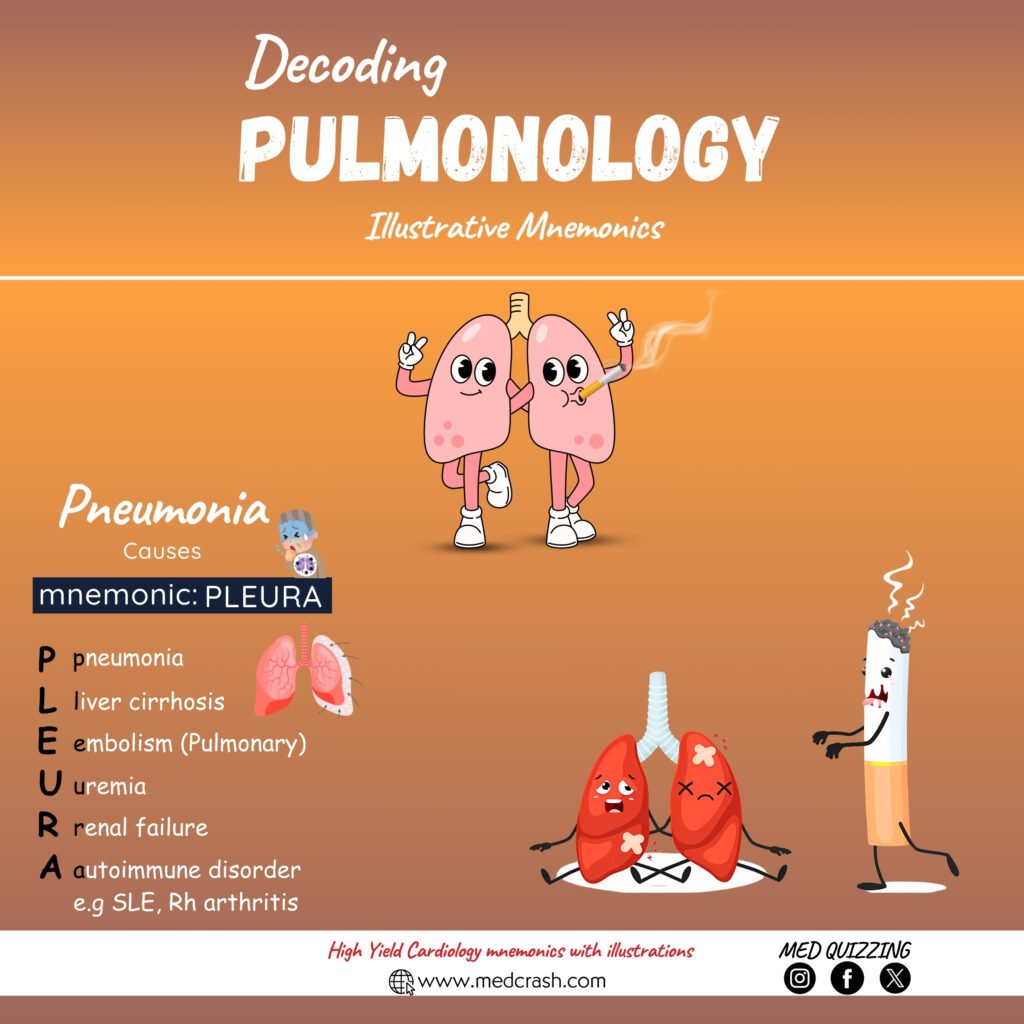
Risk Factors
- Recent infections (e.g., influenza or colds).
- Weakened immune systems (infants, elderly, HIV, or immunosuppressive medications).
- Immobility (stroke, bedridden patients, or post-surgery recovery).
- Chronic lung diseases (COPD, asthma).
- Aspiration risk (dementia, impaired swallowing).
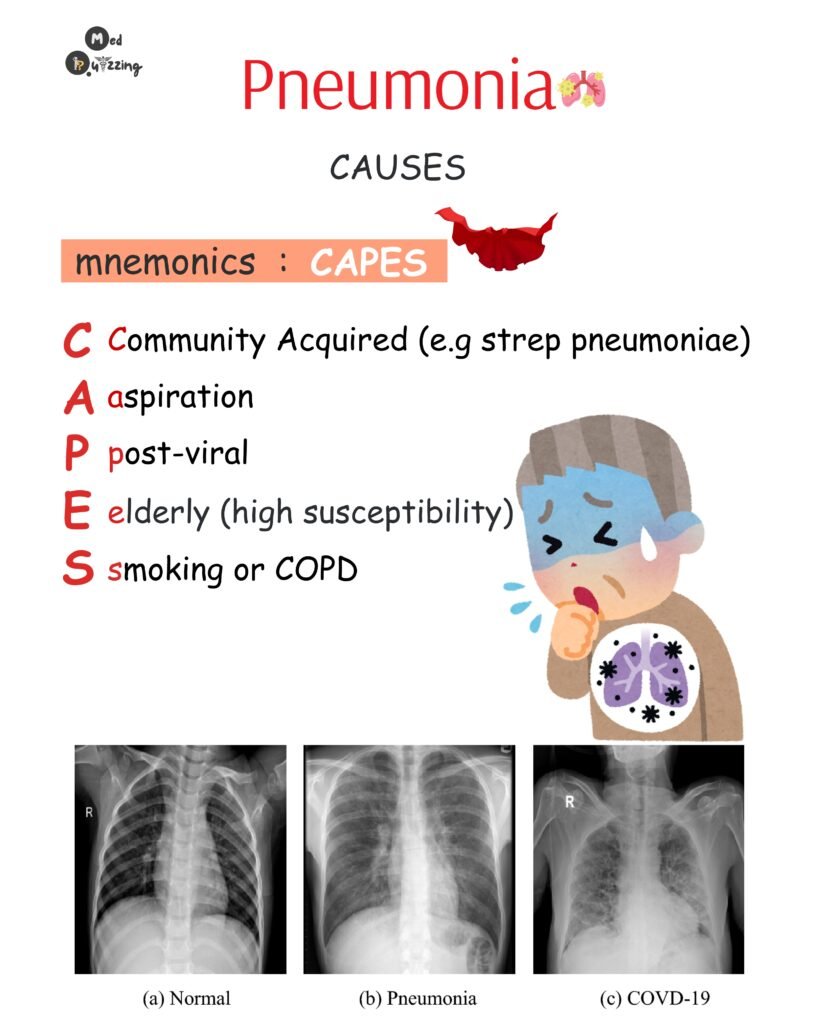
Types of Pneumonia
Community-Acquired Pneumonia (CAP):
- Contracted outside healthcare settings.
- Most common cause: Streptococcus pneumoniae.
Hospital-Acquired Pneumonia (HAP):
- Develops 48–72 hours after hospital admission.
- Often caused by antibiotic-resistant bacteria (e.g., MRSA).
Atypical Pneumonia (Walking Pneumonia):
- Caused by Mycoplasma pneumoniae.
- Symptoms are milder; patients often remain ambulatory.
Diagnosis
- Chest X-ray: Reveals lung infiltrates or consolidation.
- Sputum Culture: Identifies the causative pathogen (bacteria/fungi).
- Arterial Blood Gas (ABG): Shows respiratory acidosis (pH <7.35, pCO2 >45 mmHg, HCO3 >26 mmol/L).
- Physical Exam:
- Coarse crackles or rhonchi on auscultation.
- Bronchial breath sounds in peripheral lung fields (abnormal).
Signs and Symptoms (PNEUMONIA Mnemonic)
- P: Productive cough or pleuritic chest pain (sharp pain when breathing/coughing).
- N: Neuro changes (confusion in elderly).
- E: Elevated labs (high WBC, pCO2).
- U: Unusual breath sounds (crackles, wheezing).
- M: Mild to high fever (up to 104°F).
- O: Oxygen saturation <90%.
- N: Nausea/vomiting.
- I: Increased heart/respiratory rate.
- A: Aching muscles and activity intolerance.
Medications
Antibiotics are tailored to the pathogen and patient allergies. Use the mnemonic:
“Various Medications Frequently Treat Pneumonia C”:
- Vancomycin: For severe/resistant infections.
- Monitor: Ototoxicity (hearing loss, tinnitus).
- Macrolides (e.g., Azithromycin):
- For penicillin allergies.
3. Tetracyclines (e.g., Doxycycline):
- Avoid in pregnancy/children (tooth discoloration).
- Increases photosensitivity.
4. Fluoroquinolones (e.g., Levofloxacin):
- Risk of C. diff infection and tendon rupture.
- Cephalosporins (e.g., Ceftriaxone):
- Broad-spectrum.
- Penicillins (e.g., Amoxicillin):
- Narrow-spectrum.
Prevention Tips
- Vaccinate: Annual flu shot and pneumococcal vaccine (Pneumovax) for high-risk groups.
- Hand Hygiene: Reduces germ transmission.
- Post-Surgery Care: Use incentive spirometry to prevent atelectasis.
When to Seek Help
Seek emergency care if:
- Lips/skin turn blue (cyanosis).
- Confusion or extreme fatigue develops.
- Breathing becomes rapid or labored.
Download our Pulmonology mnemonic Flashbook