What is Hypertension? Pathophysiology, Causes, Stages
What is Hypertension?
Hypertension is the amount of resistance of blood pumping through your body and arteries. What happens is that the arteries narrow, increasing blood pressure. A helpful analogy is to think of a water hose: when you squeeze the hose, the water jets out more forcefully. Similarly, when arteries constrict, blood flows through them at a higher pressure, which can damage organs over time. This is why hypertension is a disease process that requires treatment to prevent long-term complications.
Hypertension is defined as a blood pressure of 140/90 mmHg or greater. The main goal of treatment is to decrease the risk of mortality and cardiovascular and renal morbidity.
Blood Pressure Ranges
Understanding blood pressure ranges is crucial for managing hypertension. According to the Joint National Committee, the ranges are as follows:
- Normal Blood Pressure: 120/80 mmHg or less.
- Pre-Hypertension: 120-139 mmHg systolic or 80-89 mmHg diastolic.
- Stage 1 Hypertension: 140-159 mmHg systolic or 90-99 mmHg diastolic.
- Stage 2 Hypertension: Anything greater than 160 mmHg systolic or 100 mmHg diastolic.
These ranges help healthcare professionals assess a patient’s condition and determine the appropriate course of action.
Signs and Symptoms of Hypertension
Hypertension is often asymptomatic, but when symptoms do occur, they may include:
- Headache
- Dizziness
- High blood pressure
- Retinopathy and visual changes
- Chest pain
- Sensory or motor problems
In severe or untreated cases, hypertension can lead to end-organ damage, which we will discuss later in this blog.
Systems of the Body Affected by Hypertension
Hypertension is known as the silent killer because it often presents no symptoms until it has already affected vital systems of the body. To remember the systems affected, use the mnemonic “CAKE”:
- C for Cardiovascular: High blood pressure can lead to congestive heart failure due to the overworking of the heart muscle, causing the ventricle to enlarge and pump less effectively.
- A for Brain: Increased pressure can weaken or rupture arteries, leading to a stroke.
- K for Kidneys: Renal failure can occur as the kidneys’ arteries weaken, reducing perfusion and impairing kidney function.
- E for Eyes: Increased blood flow can damage retinal vessels, causing blurred vision and difficulty focusing.
Causes and Risk Factors of Hypertension
Hypertension can be categorized into two types: primary (essential) hypertension and secondary hypertension. Primary hypertension has no identifiable cause, while secondary hypertension is caused by an underlying condition.
Risk Factors for Hypertension
To remember the risk factors, think of the word “RISK FACTORS”:
- R for Race: Black males are at higher risk.
- I for Increased Intake: High sodium or alcohol consumption raises blood pressure.
- S for Smoking or Stress: Both contribute to hypertension.
- K for Low Potassium or Vitamin D: Low levels of these nutrients can increase blood pressure.
- F for Family History: A family history of hypertension increases your risk.
- A for Advanced Age: Aging leads to artery stiffening, raising blood pressure.
- C for Cholesterol: High cholesterol levels increase the risk.
- T for Too Much Caffeine: Caffeine causes vasoconstriction, increasing blood pressure.
- O for Obesity: Higher BMI increases the risk.
- R for Restricting Activity: A sedentary lifestyle contributes to hypertension.
- S for Sleep Apnea: Snoring and sleep apnea are linked to hypertension.
Other risk factors include metabolic syndrome, diabetes, dyslipidemia, and chronic alcohol use.
Secondary Causes of Hypertension
Secondary hypertension is caused by pre-existing conditions such as:
- Coarctation of the aorta
- Pheochromocytoma
- Hyperaldosteronism
- Cushing syndrome
- Renal artery stenosis
- Chronic kidney disease
- Polycystic kidney disease
- Nephritic and nephrotic syndrome
- Obstructive uropathy
- Hyperthyroidism and hyperparathyroidism
- Sleep apnea
- Chronic alcohol use
- Use of oral contraceptives, NSAIDs, or illicit drugs (e.g., cocaine, methamphetamine)
- Preeclampsia in females
Pathophysiology of Hypertension
The pathological vascular changes in hypertension occur slowly. In normal vessels, blood flow is smooth, but in hypertension, the following changes occur:
- Early Stages: Plaque buildup and thickening of the vessel walls.
- Late Stages: Further plaque buildup due to endothelial dysfunction and hypertrophy of the vessel walls.
These changes result in the narrowing of the lumen and increased vascular pressure, aggravating hypertension. Over time, this can lead to end-organ damage, including:
- Stroke
- Retinopathy
- Transient ischemic attack (TIA)
- Left ventricular hypertrophy
- Cardiac failure
- Renal failure
Investigations for Hypertension
To diagnose and monitor hypertension, the following investigations are recommended:
- ECG (Electrocardiogram): To assess cardiac function.
- Urinalysis: To evaluate renal function.
- Serology Tests: Including plasma renin, plasma aldosterone, and thyroid function tests.
- Blood Count: To rule out other differentials and monitor hypertension.
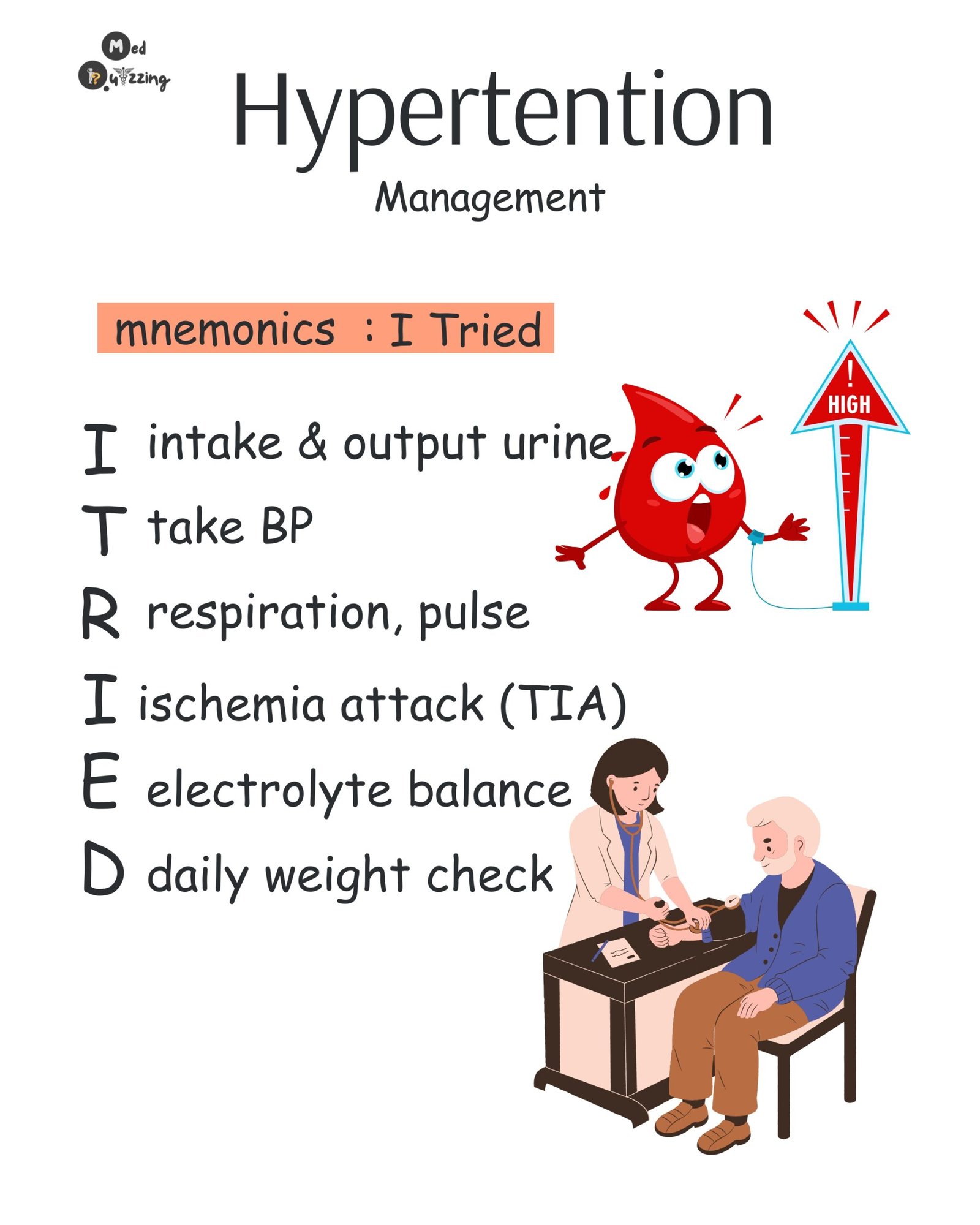
Management of Hypertension
Management of hypertension includes both lifestyle modifications and pharmacological interventions.
Lifestyle Modifications:
- Exercise regularly
- Reduce salt intake
- Follow a proper diet (e.g., DASH diet)
- Limit alcohol intake
- Smoking cessation
Pharmacological Management:
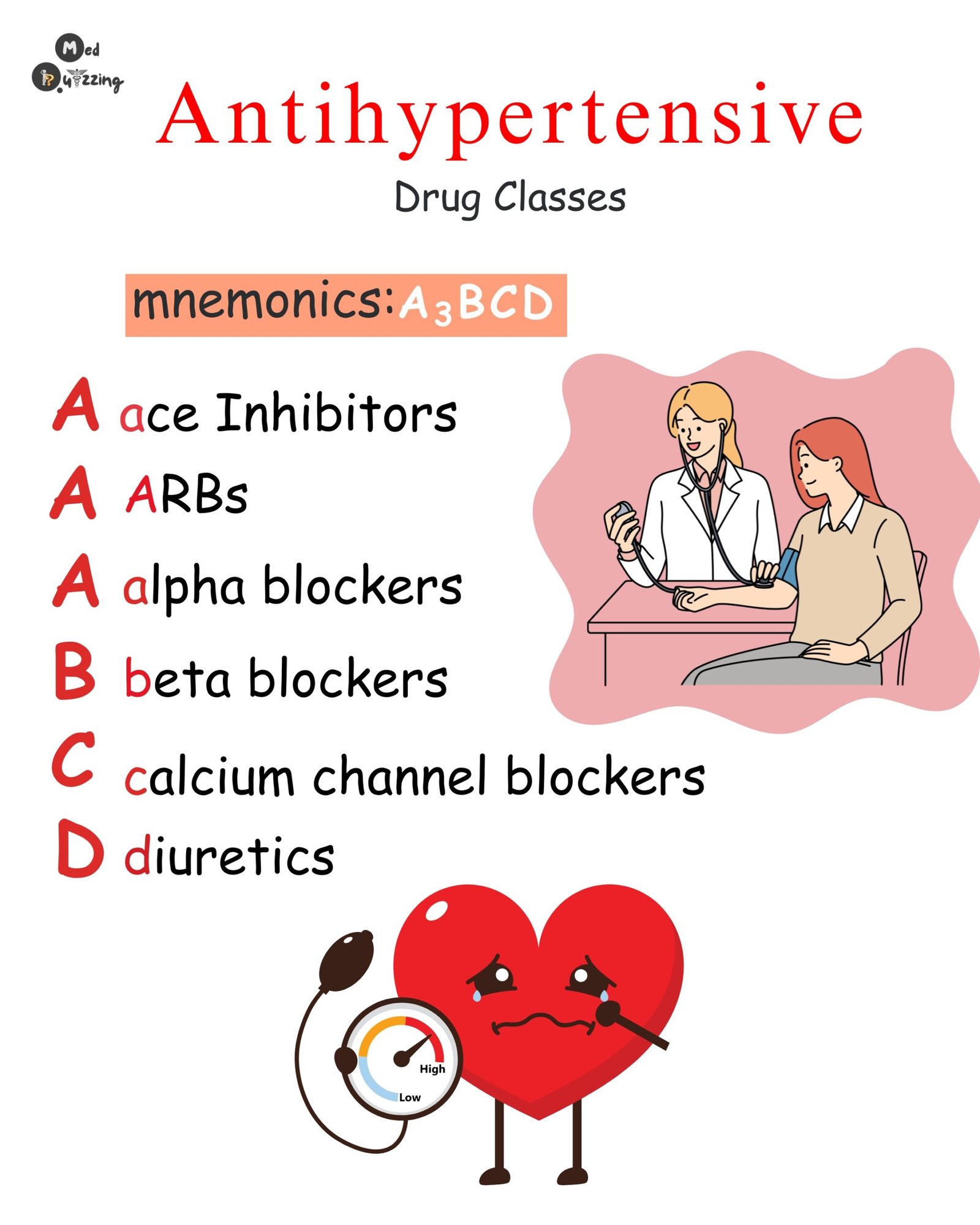
- Thiazide Diuretics (e.g., Hydrochlorothiazide):
- Work by removing water and sodium through the kidneys.
- Educate patients about potassium supplementation and photosensitivity.
- ACE Inhibitors (e.g., Lisinopril):
- Prevent vasoconstriction by blocking angiotensin receptors.
- Side effects include a dry cough and potassium retention.
- ARBs (Angiotensin Receptor Blockers) (e.g., Losartan):
- Block aldosterone and angiotensin receptors.
- Used as an alternative for patients who cannot tolerate ACE inhibitors.
- Calcium Channel Blockers (e.g., Amlodipine):
- Lower heart rate and cause vasodilation.
- Monitor for bradycardia and avoid use in patients with heart failure.
- Beta Blockers (e.g., Metoprolol):
- Block epinephrine, reducing heart rate and blood pressure.
- Avoid in patients with asthma or COPD, and monitor diabetics for masked hypoglycemia symptoms.
Patient Education:
- Limit sodium, alcohol, and caffeine intake.
- Encourage smoking cessation and regular exercise.
- Teach patients how to monitor their blood pressure at home and keep records for doctor visits.